Determining if a person who presents itself with pain in the chest suffers from a myocardial infarction or ACS (Acute Coronary Syndrome) is an everyday challenge in emergency departments and physicians are working with standard diagnostic instruments such as the troponin test and ECG, to conduct this assessment.
In the past years tremendous progress has been made in this field and the risk assessment is getting better and better. And this safes both lives and costs because the classic solution of admitting patients into hospital, run some tests and monitor the heart performance was not really supporting increasing patient outcomes. A significant part of this progress can be allocated to the introduction of high sensitive troponin tests. This blood test which looks for a specific marker related to a hart infarct incident used to take at least a day before results came in from the lab. And this was needed since the existence (and traceability) of troponin increases in the hours after a cardiac incident which requires the physician to wait before the classic troponin test indicate values indicating an MI incident and thus treatment. And during this waiting time patients get other tests (such as CT, X-ray, stress tests). With additional risks as a consequence. In an article by Anton Helman on this issue, in which he introduces hs troponin tests as the new frontier, he says: “we tend to underestimate the risks of admitting patients to the hospital as well as the risks of overdiagnosis”.
High sensitive troponin tests are game changers
With the introduction of high sensitive (HS) troponin test this waiting time can be significant reduced. With the current protocol suggesting to wait at least 3 hours after the pain in chest symptoms started to occur before the test taking or to apply at least 2 HS troponin tests with a minimal interval of 2 hours to verify if there’s a change in the troponine levels.
This is needed because there’s always troponin produced by the human body and this level differs per person.
Initial assessment is broader than a troponin test
Troponin is not the only indicator used in this MI determination process. The so called HEART approach which stands for History, ECG features, patient Age, ACS Risk factors and Troponin recognizes 4 other patient aspects which should be taken into account. But the recent availability of the HS troponin tests has changed the balance in these assessment factors. And recently we saw the presentation of study results, supported by a a handheld rapid HS troponin test device, which suggests the HS troponin test could be applied by para-medics and could influence the decision to yes or no take people with pain in chest symptoms to hospital and the ER.
Given the early description of ‘how to effectively use a hs troponin test” and apply either a 3 hour initial test threshold or apply 2 tests with an interval of >2 hours, this solution should require an ambulance to wait for hours before taking a person to hospital which is not really effective (if the ambulance is already on the patient location).
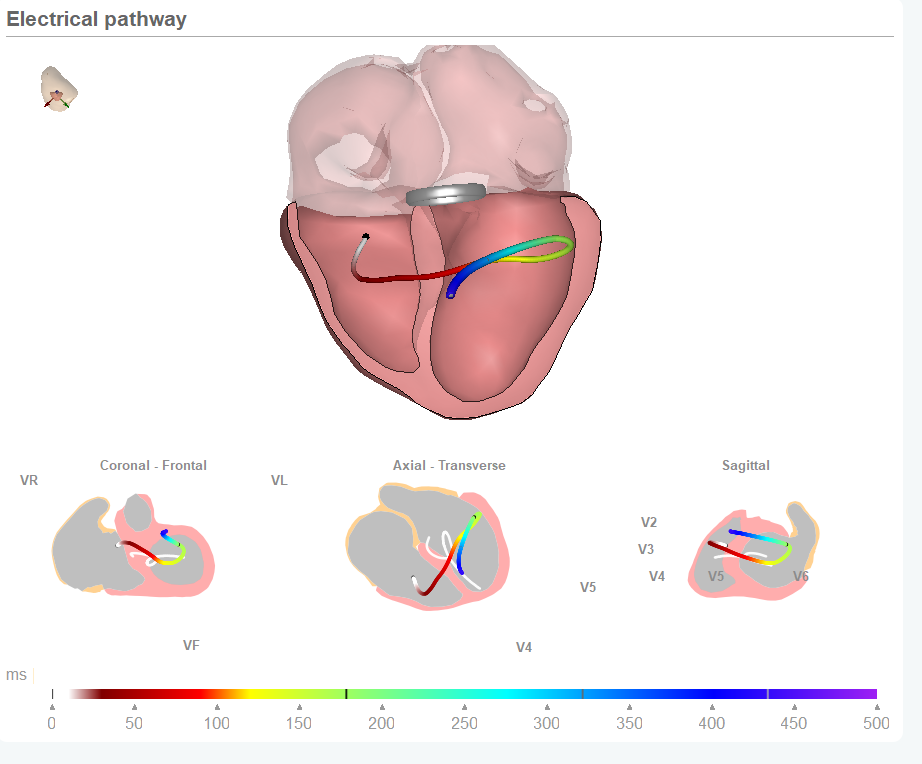
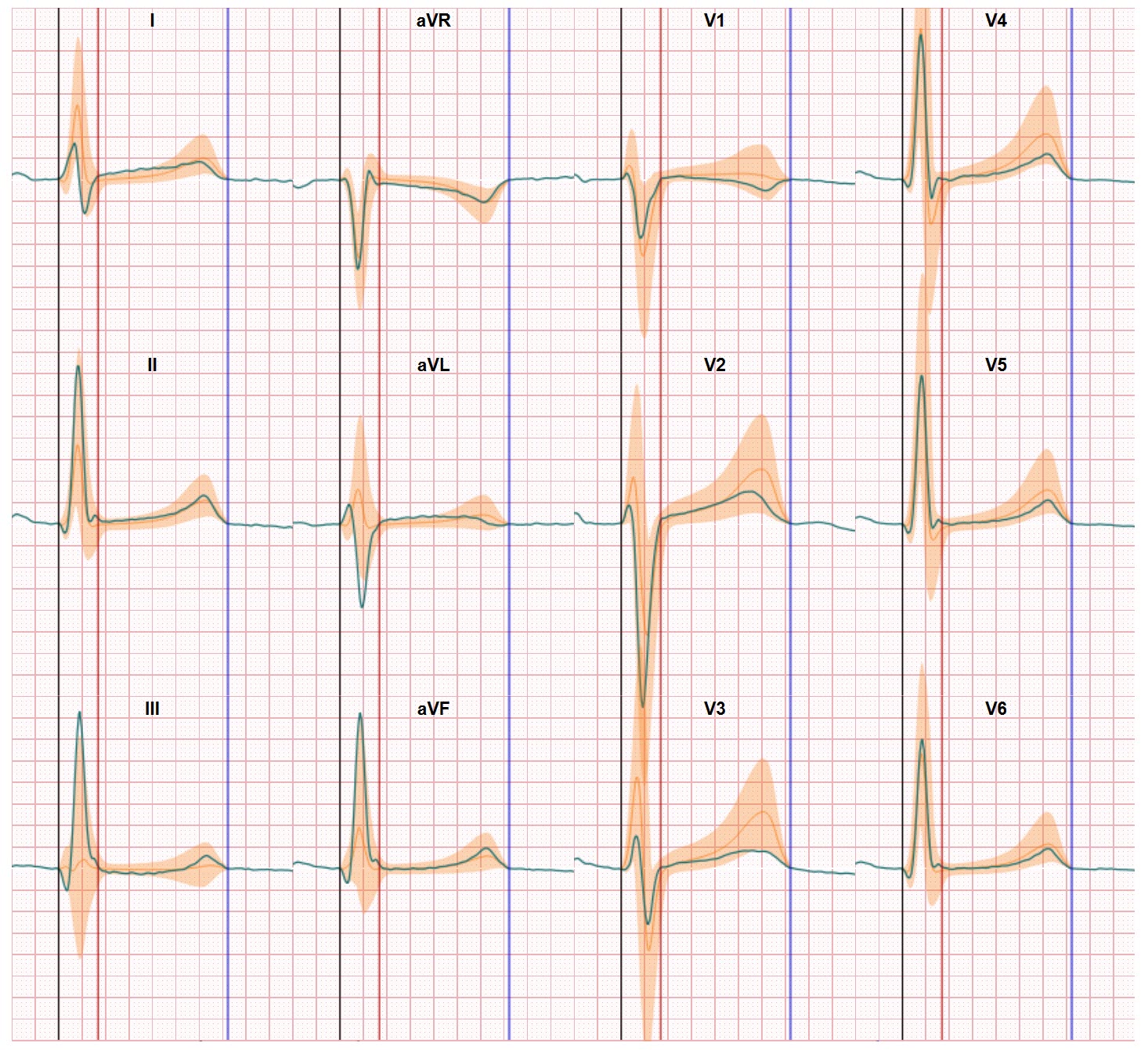
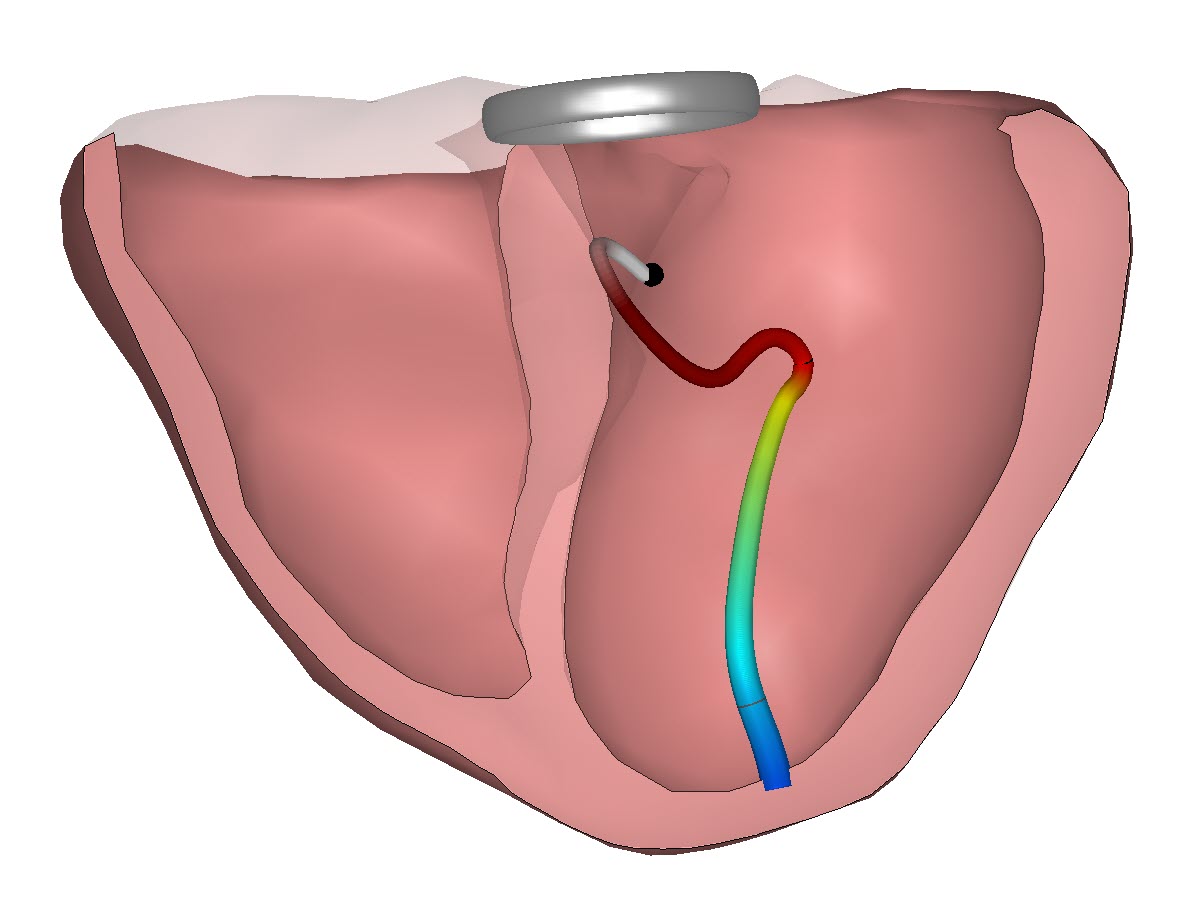
Improved ECG interpretation might be the next way forward
Besides innovation in troponin testing there’s another route for improving pain in chest assessments. Where today the ECG features in the HEART protocol are focusing on determine if the ECG is normal to support a non-MI decision, we think there’s much more to see in the ECG and the balance between the troponin test and ECG in initial pain in chest assessment. After a MI incident the electrical pathway shows a different pattern and there’s no need to wait for hours to determine a high or changed troponin level to already identify a cardiac disorder. With a novel technology such as CineECG the difference between the recorded ECG and a normal ECG is immediately shown and the troponin test can be used for verification of the ECG based finding. Recent study results indicate CineECG in its current basic form classifies +25% patients with ACS just from 12 lead ECG data and this can be a real time saver reducing patient waiting time, diagnostic efforts and ED staff time.