There’s a lot of progress in heart disease detection! But how to measure this progress. An interesting approach is to look at the objectives mentioned during an inaugural speech of a professor in Cardiology (in Dutch only) some 20 years ago. In this case prof. dr. Martin Schalij of Leiden University in The Netherlands. A university with a reputation in Heart disease diagnostics since this university gave birth to the Electrocardiogram technology in 1911. At the time of his speech in 2003 prof. Schalij reflected on the relative low level of innovation which had characterized Cardiology and suddenly had turned into a whirlwind of new options for treating critical heart arrhythmias. Schalij focused his contribution on reducing the occurrence of sudden cardiac death. Especially the introduction of the implantable cardioverter defibrillator (ICD) and the introduction of catheter ablation provided new treatment options. And based on this optimism he mentioned 3 key focus area’s for further improvement:
- Addressing patients with genetic heart diseases or patients with heart diseases from birth.
Understanding their disease progress and measuring treatment effectiveness are true challenges for the future (as seen in 2003) - The origins and development of Atrial Fibrillation because the impact of Afib was becoming more clear where the cause of Afib was still to be investigated. In his speech Schalij hinted on conduction disorders as a probable cause;
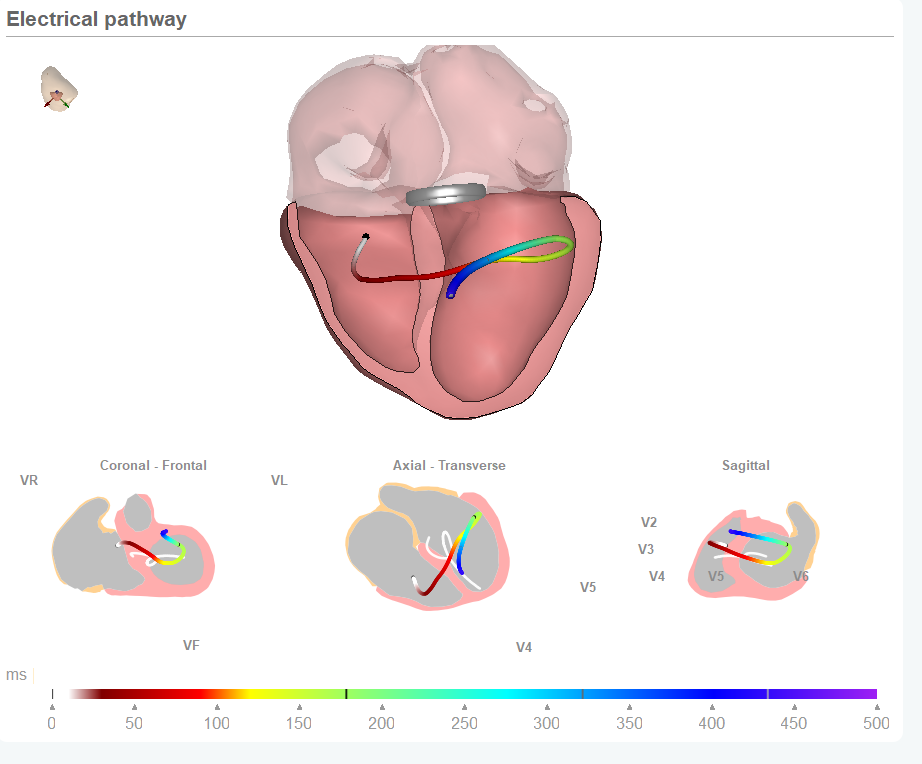
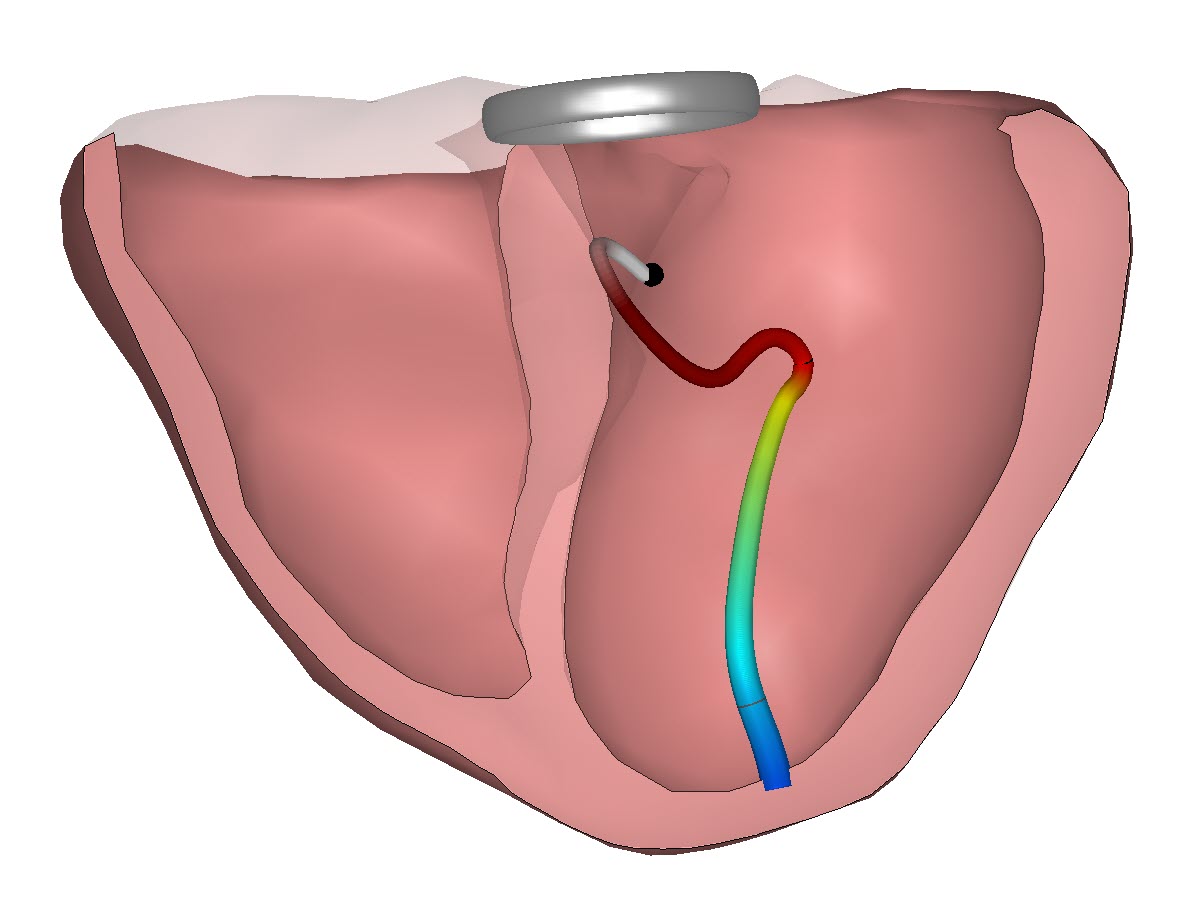
- Cardiac mapping to visualize what is happening inside the heart and to support both the monitoring of disease progress, the placement of ICD wires and to indicate where to ablate.
Making slow progress in heart disease detection
Almost 20 years have passed since this vision on the future challenges. And if we take a look at the progress we can only conclude all the questions and challenges are still relevant. We have made progress on identifying genetic heart diseases, we have further modernized the interventions in the catheter lab and we have moved in 3D mapping. But science and industry did not solve all the puzzles.
The heart is even more complex than expected and still comparing a person’s heart performance over time and thus track progress of disease or treatment is a challenge. Atrial Fibrilation has gotten a lot of attention but understanding the preceding tissue changes is still being investigated. And cardiac mapping is both expensive and cumbersome. Non-invasive body surface mapping requires a lot of electrodes and CT scans, invasive catheter based mapping is expensive and not available as an easy rapid screening tool.
12 lead ECG provides new options
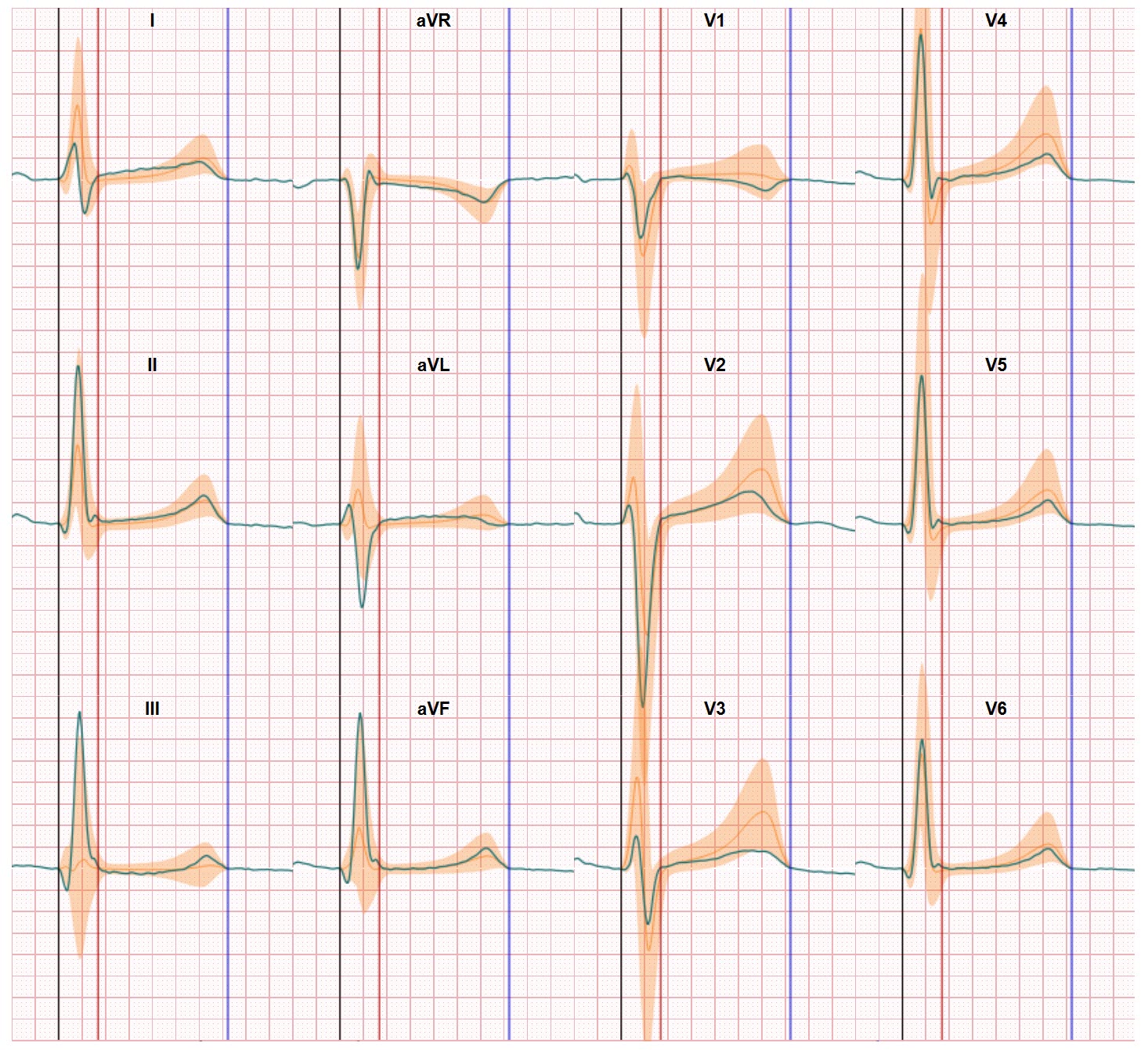
All this progress is impressive but the still open challenges require new approaches. We see the appearance of Artificial Intelligence as positiv,e but from our side we think the back to basics route is probably even more fruitful. If you take a higher level look at prof. Schalij’s remarks in 2003 you see the clear need for better insights on what’s really happening within the electrical activation and recovery processes in the heart. And this is where moving the classic 12 lead ECG to the digital age through computerized modelling provides new options for making progress in heart disease detection.