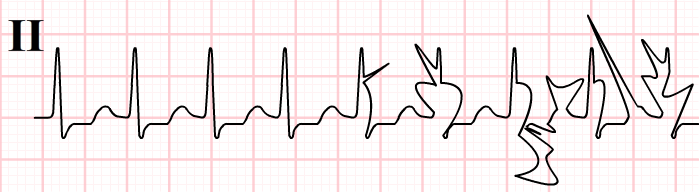
Rapid and correct ECG interpretation is essential in Emergency Departments, mistakes in ECG interpretation should be avoided if possible. Electrocardiograms are in the list of most used diagnostic tests in the first line care and not without reason. An ECG or EKG is fast, non-invasive, low cost and looks easy to conduct. Just watch the numerous ER type of television series and the ECG is often the most used word when an new patient enters the scene. Patient lives
And yet, doctors struggle with ECG interpretation. In a 2016 article by Fairley and others regarding ECG interpretation in emergency rooms the figures are worrying. Non-cardiologists, which these physicians often are, have an accuracy of 36% to 96% in detecting ECG abnormalities and even acute myocardial infarction is missed in the assessments.
And the consequences are significant. Not only has research demonstrated ECG analysis and interpretation have an impact the Emergency treatment of a patient in 32% of the cases. Also mistakes in ECG interpretation result in mismanagement of patient in 11% of the cases. With various results of course.
Reasons for making mistakes in ECG interpretation
In the emergency setting patient evaluation needs to be done rapidly. Fairley and his co-authors focus on the process of ECG interpretation within the ER context to search for improvement options. They highlight the focus on looking for STEMI patterns (ST elevation) and actually shifting a more detailed analysis of the ECG to a later stage when the STEMI patterns are not seen. They also mention the lack of patient history within the ER context and the need to compare the patient ECG preferably with earlier ECG recordings or apply serial ECG recording during the ER visit.
Another factor mentioned is the use of the computerized ECG analysis from the embedded software in the ECG devices. The accuracy of these algorithms is poor and the average accuracy for ECG waveform analysis results is near 50%. In order to reach at least a acceptable professional ECG interpretation you need to train and make the hours like a chess master. In their article a volume of at least 3500 ECG analysis is mentioned as a entrance level.
Poor ECG interpretation is a fact of life apparently and the lack of an effective set of well define criteria to determine yes/no in ECG interpretation is a cause in the mistakes in ECG interpretation.
Reducing mistakes in ECG interpretation
Apparently the authors accept the decennia status quo regarding the ECG technology and the way ECG interpretation is conducted. The article refers to the fact that it is common for cardiologists, electrophysiologists and emergency physicians to have a poor rate of inter-rate reliability when viewing the same ECGs. Even when the same physician looks at an ECG dataset over time the interpretation may differ.
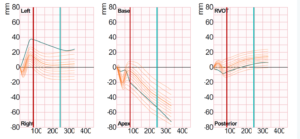
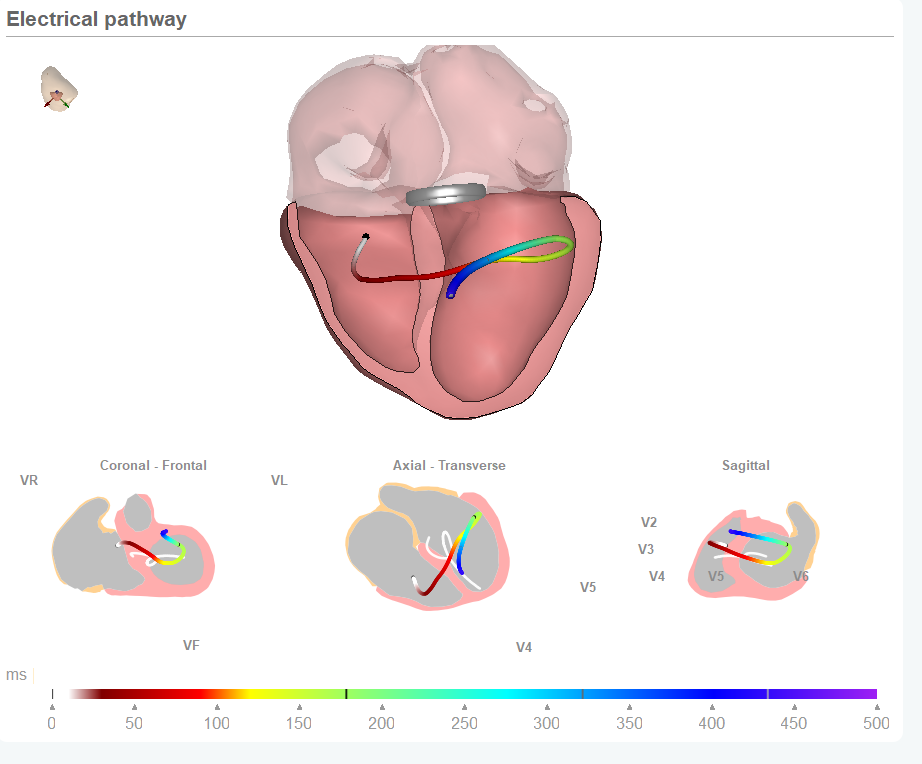
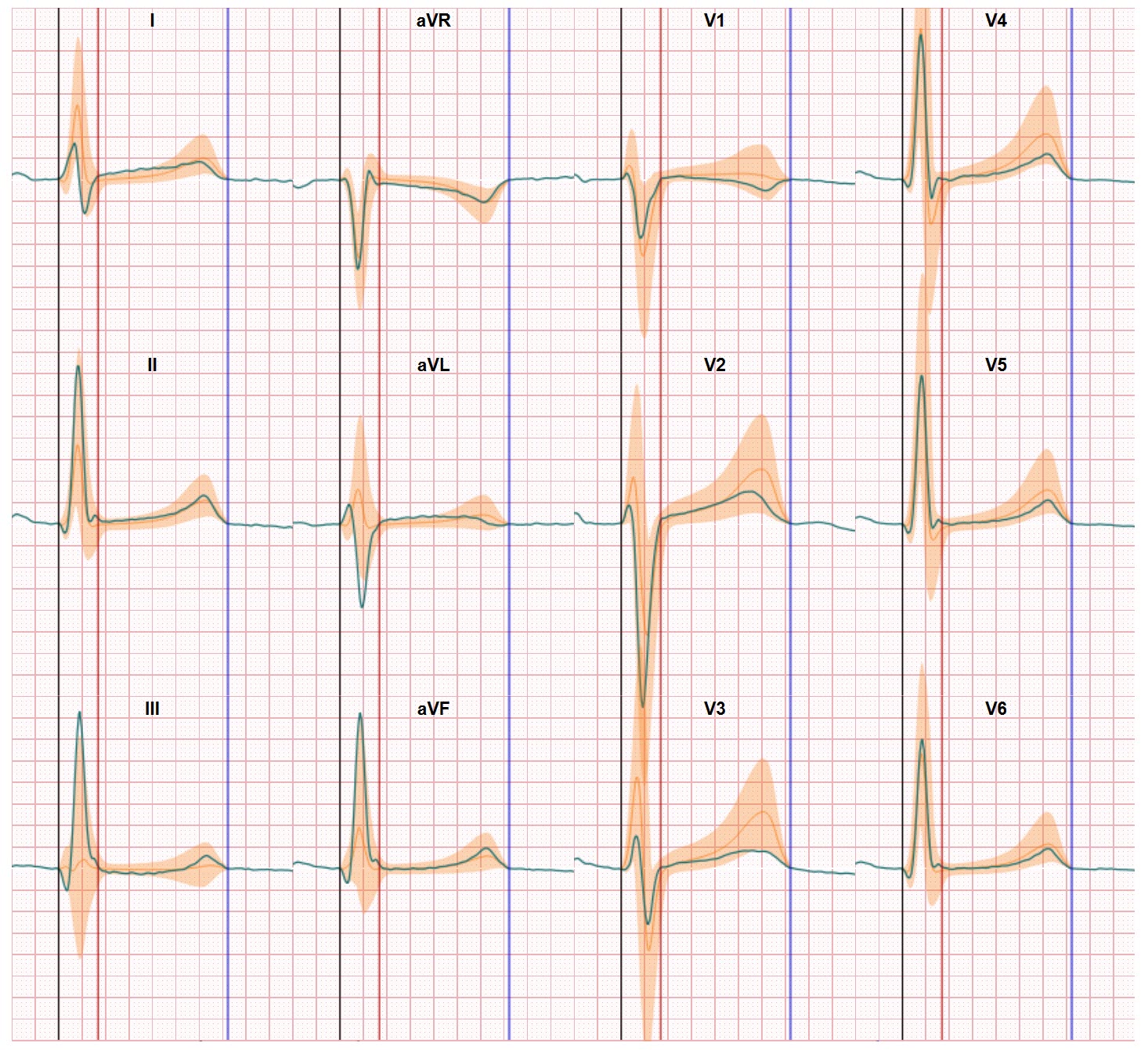
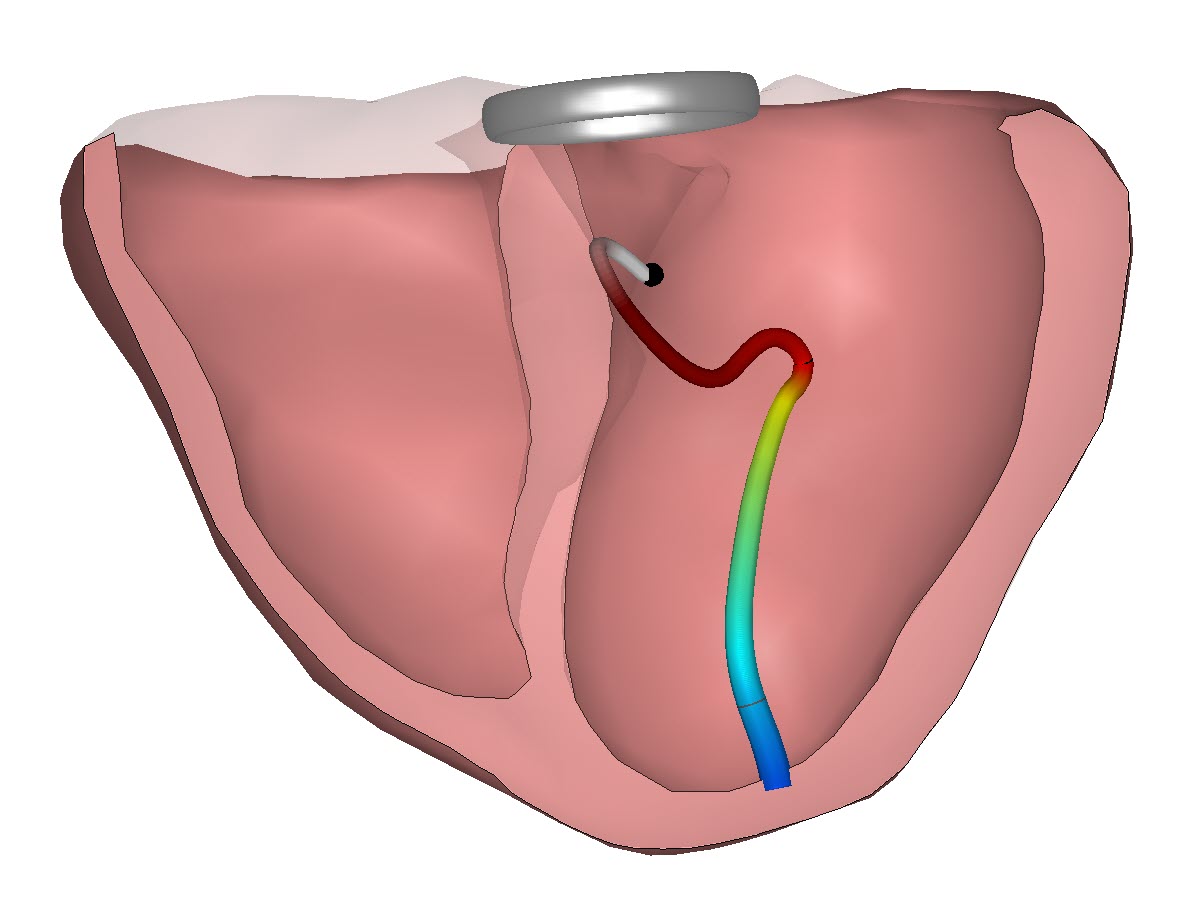
As a company and as a team driven by the passion to reduce mistakes in ECG interpretation we know the majority of these ‘mistakes’ can be avoided. And changing the way we work with ECG data is the key. The classic 12 lead ECG output is a set of 12 graphs which have to be evaluated simultaneously. The physician should be able to convert the 2 dimensional data to the 3 dimensional world of the heart anatomy and then be able to spot abnormalities. In a world where pattern recognition is the focus of training this is alas a vanishing skill.
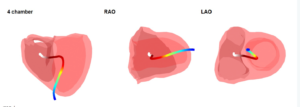
This is where the CineECG technology offers support. The ECG data is presented in different views in which the relationship with the heart anatomy is visualized and the ECG data are compared with normal values both in the electrical path through the heart and the amplitudes. Accuracy in determining yes/no is lifted close to 100% and patient management in ER settings can benefit. More information can be found here.