Although the Electrocardiogram was introduced to the medical profession over a 100 years ago Learning ECG interpretation skills is still a major challenge for physicians. Today the original 3 electrodes which were introduced by Professor Willem Einthoven have today been replaced by 10 electrodes (but less electrodes can be used if you only focus on heart arrythmia analysis), of which 6 need to be placed at specific positions on the torso. In the past century the base technology for ECG has hardly changed. Electrodes record electrical potential differences on the skin and show the differences between 2 electrodes in the formal of a graph. The main source of the electrical activity within the body is the heart and given the positions of the electrodes against the heart the ECG graph shows if the activation is moving away or towards a specific electrode. This is reflected in the value of the ECG waveform which is either plus or minus (against the base line within the graph). Over the century more electrodes have been added, the positions on the torso have been recommended, the ECG paper has been standardized (to enable measurements against the X axis for time) and Y axis (for voltage), we have improved amplifiers and converted the recorded signal to digital data.
And despite all these improvements the average accuracy in 12 lead (10 electrodes) ECG interpretation amongst physicians is only 54% correct.
In a recent article in the journal of Electrocardiology Breen and others write: “it has been reported that up to 33% of ECG interpretations contain errors of major importance. Interpreters of ECG tracings (i.e. physicians and other readers of the ECG) do not always have a high degree of intra and inter-rater reliability. Routinely cardiologists correctly identify abnormalities between 53% and 96%. And non-cardiologist interpretation, correct identification falls to between 36% and 96%.
In their root cause analysis Breen suggests that the reported differences and errors in ECG interpretation accuracy can be related to the training background of the medical professionals.
And in their research to have conclude “there remain no established standard methods for teaching ECG interpretation or reporting ECG findings that are evidence based”. Within the literature Been studies, teaching of ECG interpretation mostly occurred through lecture formats (75–90%) supplemented by small group practical teaching (44%–78%) with ECG interpretation rehearsal representing the main learning activity.
And besides this formal educational approach we now see a fast growing presence of Social Media based ECG interpretation offerings. But within the hundreds of books, video’s other posts we still see the ubiquity and variety in ECG interpretation approaches and results. And computer assisted ECG interpretation has not delivered results on average which outperform the human based interpretation. Although the recent arrythmia focussed applications show an increase accuracy performance this is still not the case for conduction and waveform analysis.
Alternative to improving learning ECG interpretation skills
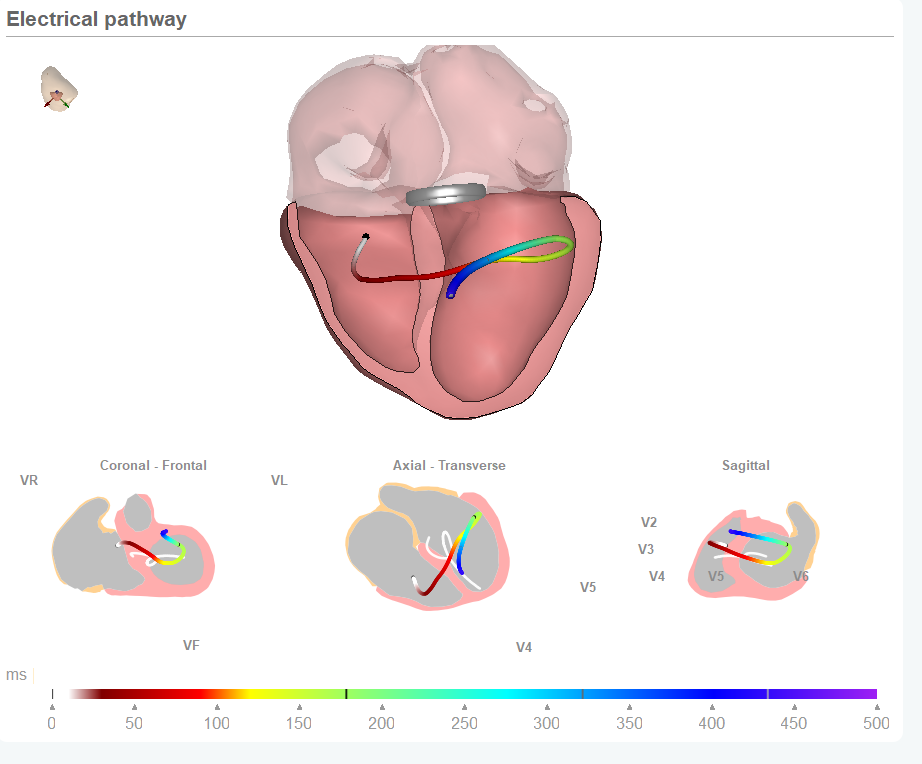
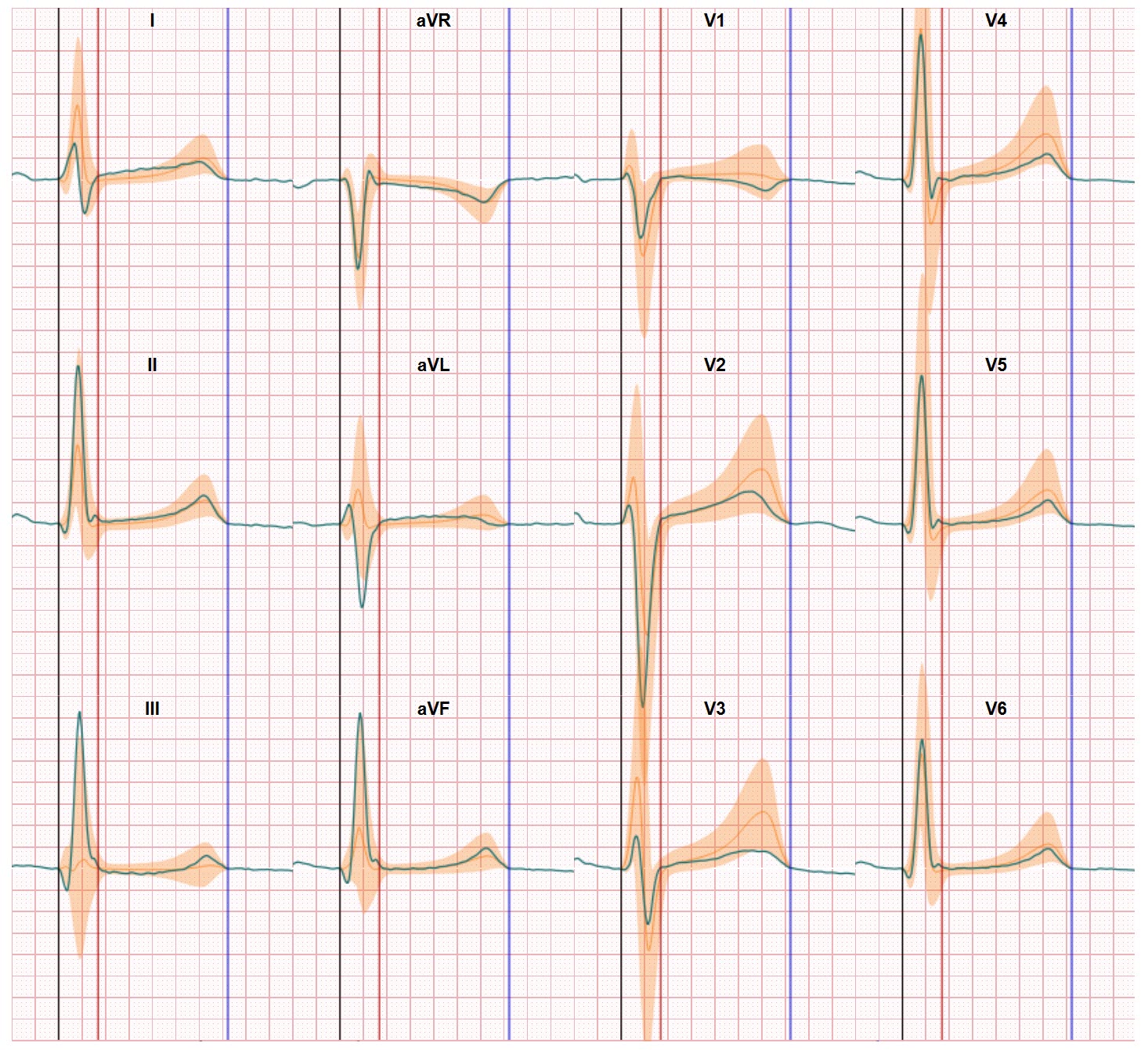
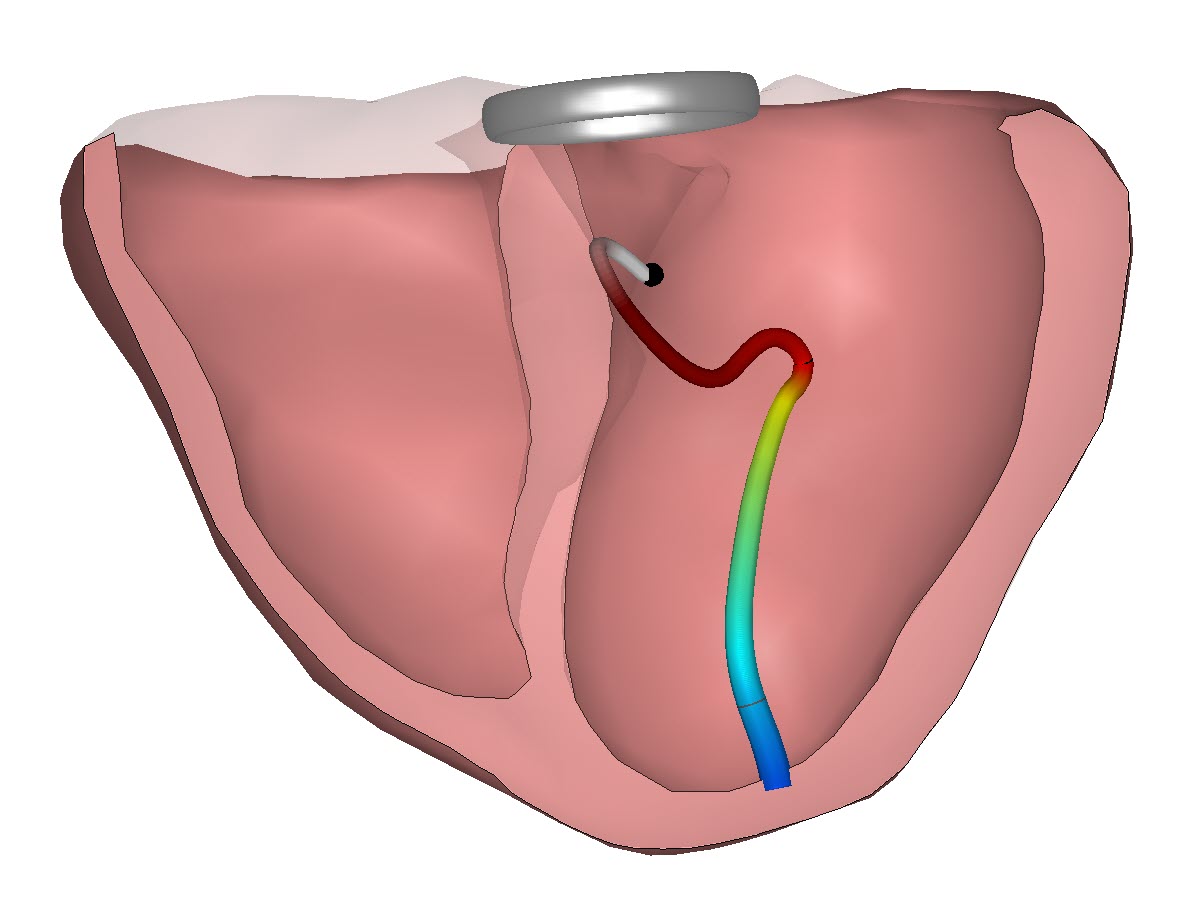
Of course Been is correct in his findings and the solutions which follows from his finding. But all their findings and solution suggestion safely remain within the boundaries of the classic ECG technology as introduced by Einthoven. Learning ECG interpretation skills is still based on ‘reading’ the ECG graphs and trying to relate these graphs to the heart anatomy or just memorize ECG graph patterns which are qualified as abnormal. And over the years we have learned that is still trying to master a complex art. Our team thinks we have to go deeper into changing the basics of ECG data presentation to make ECG interpretation easier and also simpler to learn. This can be achieved (and is achieved) by taking digitisation also further and support the physicians in relating the ECG data to the heart anatomy, by visualizing the activation pathways through the heart and by showing the differences between recorded ECG and normal healthy ECG values. Standardizing the output reduces the variability in the ECG input (heart orientation, electrode positions, body build) and will support standardized training and education in learning ECG interpretation skills.