Genetic heart disease diagnostics improvement is a true challenge for physicians. Often the first manifestation of diseases such as arrhythmogenic cardiomyopathy (ACM) are a significant drop in heart performance (heart failure) or a lethal rhythm disorder in a large heart chamber. Early signs and symptoms may be subtle and go unnoticed when interpretating an Electrocardiogram (ECG) Physicians are in great need of appropriate screening and risk-stratification strategies.
In a recent publication in the Journal of Electrocardiology a Dutch study (in which our scientific director participated) evaluated three new methods to provide information on the disease progression and the risk classification.
The first method is Isopotential Mapping. In this approach so-called body surface potential mapping is conducted using 67 or more electrodes. In this approach just using 12-lead ECG with 10 electrodes produces insufficient data to derive conclusions on genetic disease progression. Using more electrodes and thus a higher resolution increases the probability to identify abnormalities in the ECG. In this approach CT or MRI based anatomical models of the heart are used to register the heart position and the electrode positions.
The second approach is called non-invasive local activation timing mapping. Again this requires the Body Surface Potential Mapping technique combined with CT or MRI imaging. The result is a further insight into the performance of the heart activation through voltage maps. In this approach a reconstruction of the heart activation in the large heart chambers is executed. And it offers the option to reconstruct both the inside and the outside of the heart when a so-called double layer model of the heart is used. This approach can really help in early identification of heart disease and also in disease progression registration. But it works best if the heart is still ok and the results may be impacted because the difference between a normal heart model and the actual heart tissue becomes too large.
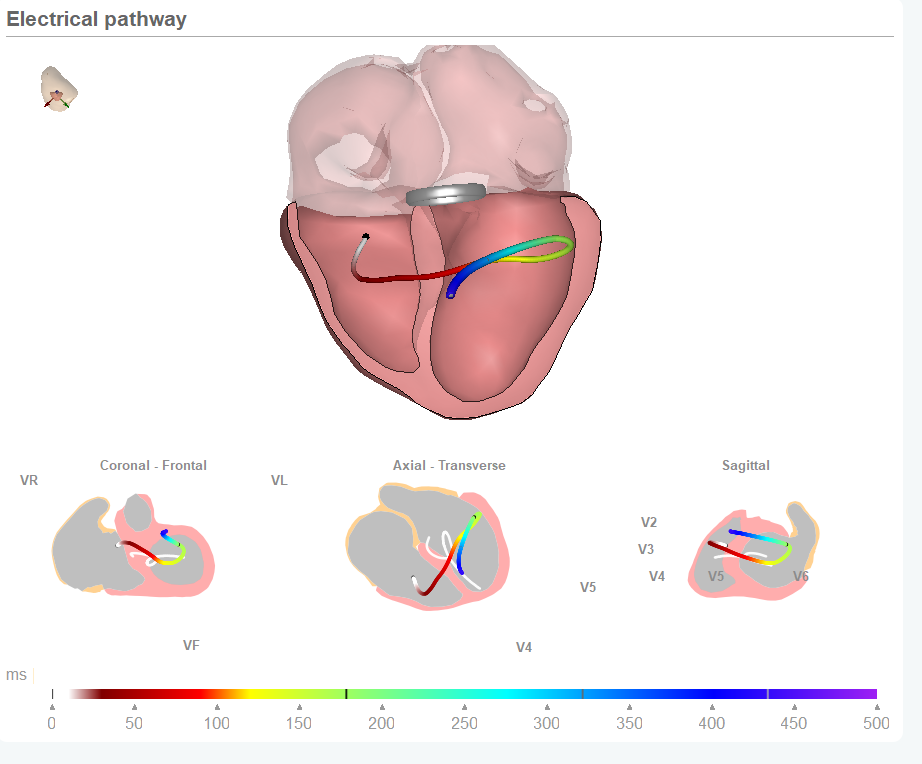
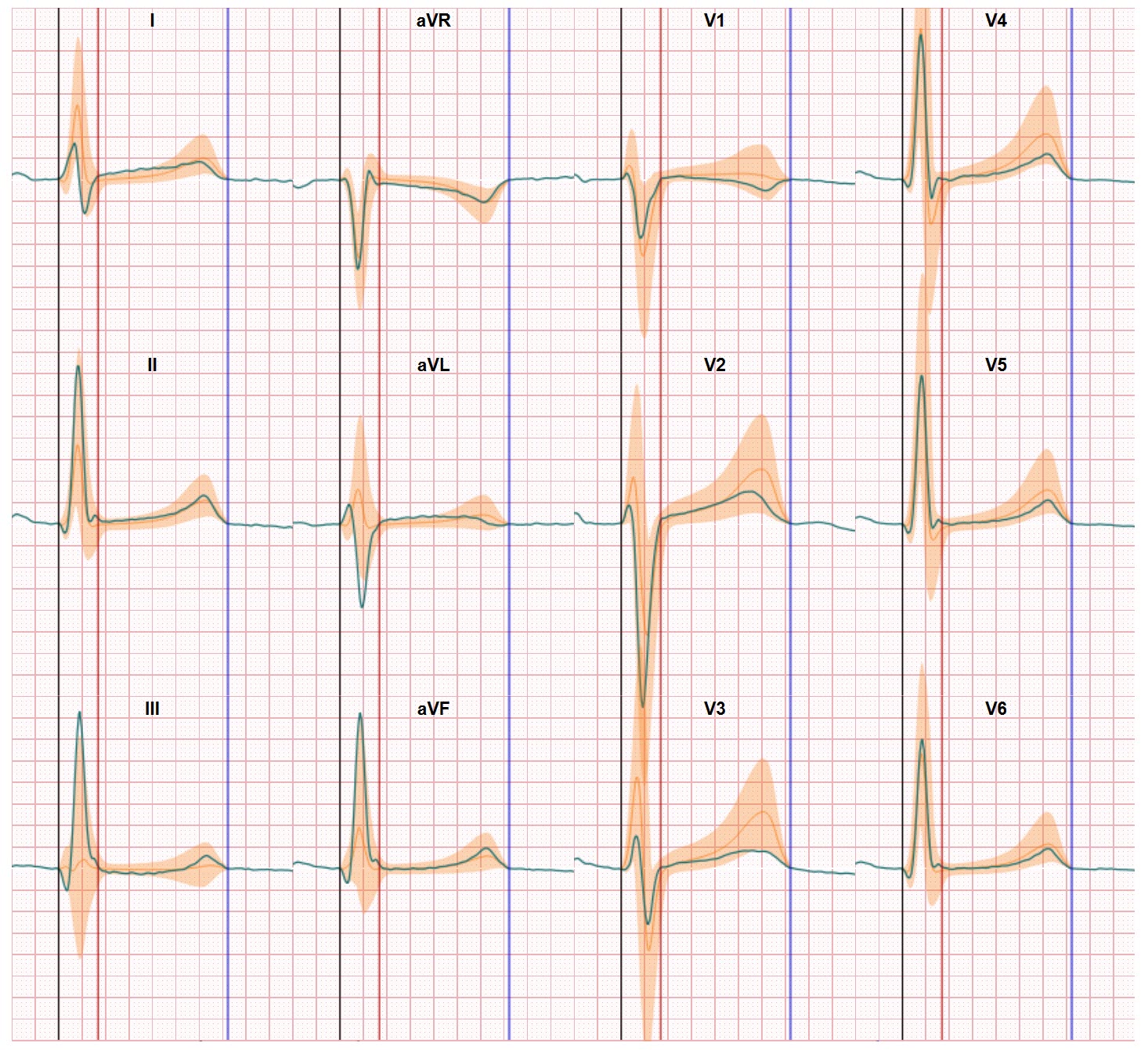
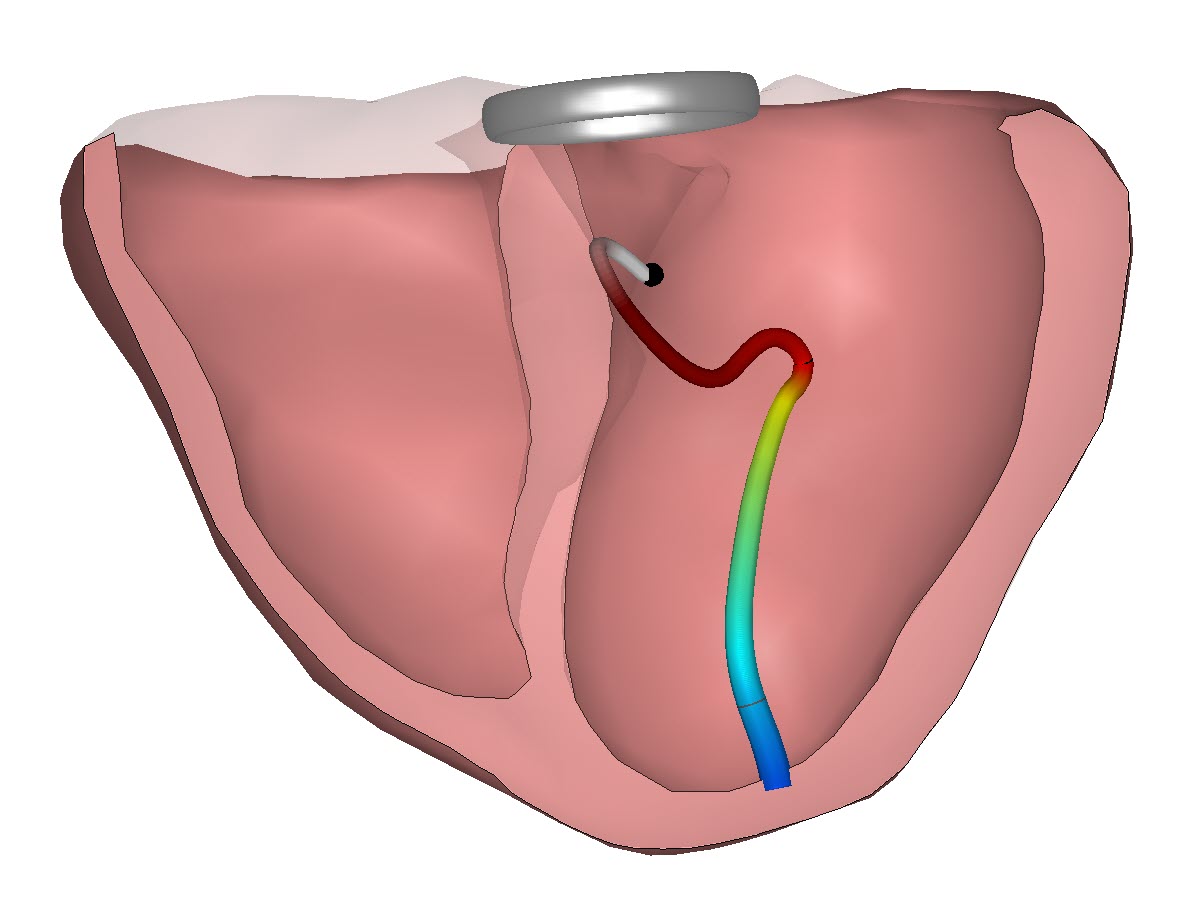
The third method in the study is CineECG. In this approach the average electrical pathway of the heart activation is derived from standard 12 lead ECG data and related to the heart anatomy. CineECG in its basic form does not need additional patient specific data derived from CT or MRI imaging. The CineECG technology supports detection of subtle abnormalities in cardiac activation and recovery which go unnoticed in the standard 12-lead ECG.
And the conclusion of the study speaks for itself:… early electrical signs of disease progression may be identified prior to symptoms… and … individualized risk-stratification may be enhanced….
For numerous patients CineECG can help to reduce the uncertainties when they are diagnosed with a genetic heart disease and their doctors get the insights to start appropriate therapies in time. And with only using standard 12 lead ECG data the execution remains within the clinical work flow and does not require additional imaging or time consuming BSPM procedures.
We thank the researchers for their work and continue our quest for genetic heart disease diagnostics improvement and related patient support.