Heart disease diagnostics based on 12-lead ECG is difficult but Female heart disease diagnostics appears to be even more challenging. Female hearts are different from males and this also reflects in differences which can be seen in the electrocardiogram. These difference relate to both the timing of specific intervals within the heart activation cycle but also the amplitudes (potential differences registered) are larger in males than in females. More details to be found in the this article from Dr Moss in the annals of noninvasive electrocardiology. Differences in heart tissue thickness also influence the recorded ECGs. And these differences also are relevant in diagnosis of heart diseases. For instance, accurately diagnosing subtle ischemic-related ECG changes in women.
Another issue is the accuracy of ECG electrode positioning which differs between males and females. The recommended 12-lead ECG electrode positions have been derived from male torso’s and differences in ECG electrode positions also impact the ECG waveforms. There are limited studies in this domain but the available data suggests in female ECG recordings one or more pre-cordial ECG electrodes (the ones closest to the heart) are misplaced in 80% of the ECG recordings. For males this number is also high (50%) but at least less impactful.

Female ECG normals is another issue
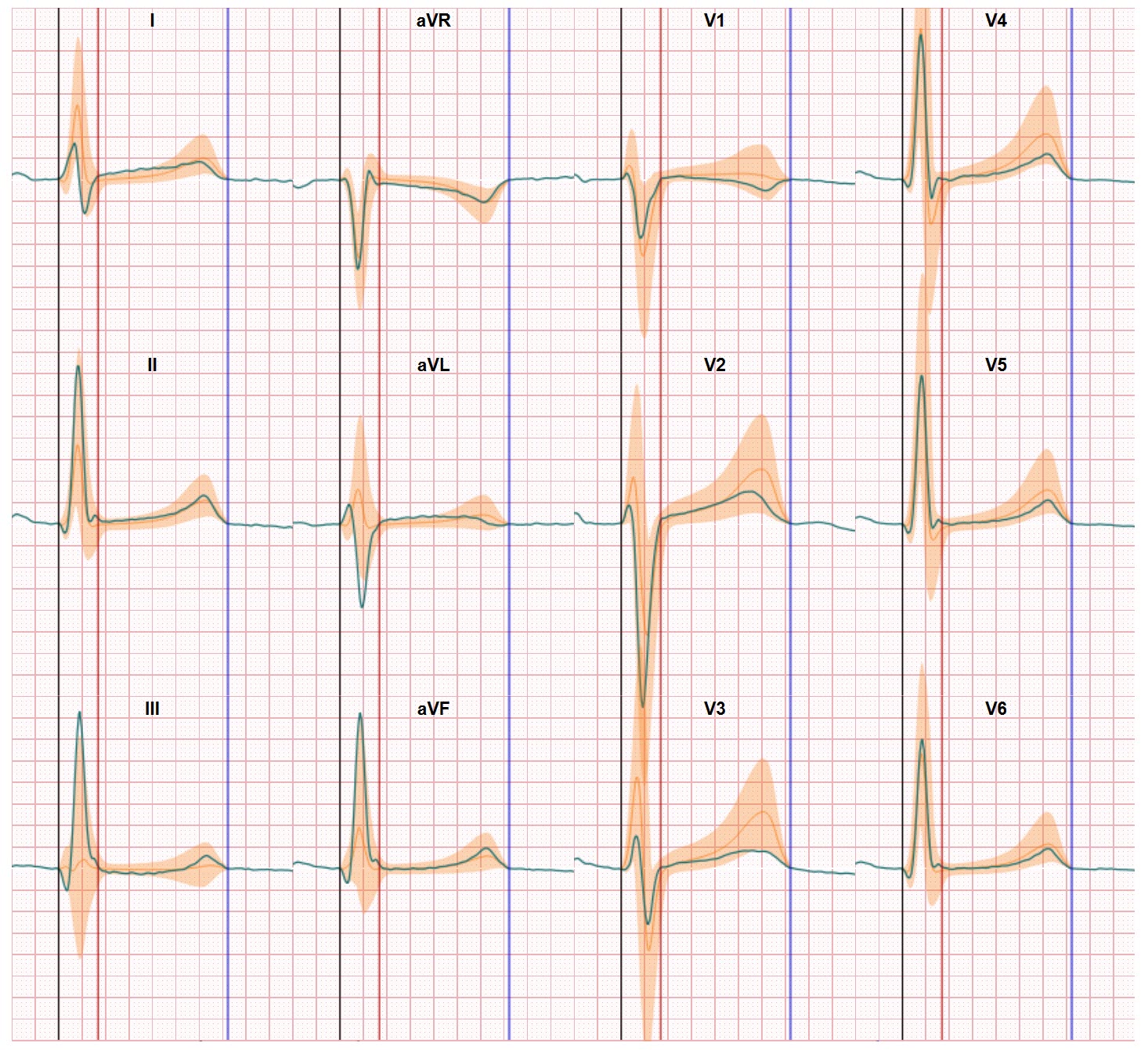
Recently we ran into another example of the challenge of distinguishing between normal and abnormal electrical heart performance when we focused on female heart disease diagnostics with our technology which compares recorded ECG waveforms with a normal distribution of healthy persons ECGs. For our research we used a database of 23000 qualified (evaluated by cardiologists) ECGs (PTB-XL database). Within this database the composition was around 52% Male ECGs and 48% Female ECGs. And from this database we selected the ECGs which had been qualified as Normal.
This selection showed a remarkable balance between normal ECGs from males and females. 59% of normal ECGs were from females and only 41% was related to males.
From a statistical point of view an unexpected result. If this reflects standard practice, and we have nor reason to doubt this, given comparable results from other databases, the probability of your ECG being evaluated as normal is much higher if you are a female. For our team this is another indicator we need to focus much more on highlighting the differences in male and female normals in ECG interpretation. Female heart disease diagnostics can this way be improved significantly