Chest pain is the most common manifestation of coronary heart disease and almost always physicians use the ECG to diagnose chest pain. Patients with Angina Pectoris (as it is called) feel an oppressive, pressing or oppressive feeling in the middle of the chest. With a gradual narrowing, chest pain occurs especially with exertion or with emotions; at rest it goes away. This is the stable form: called stable angina pectoris. Myocardial infarction is the acute form.
In case of (suspicion of) stable angina pectoris the immediate need to act is not present and further research is done: risk stratification and, if necessary, diagnostics. Upon confirmation of the diagnosis of stable angina pectoris, targeted treatment (medications and, if necessary, surgery) and cardiovascular risk management (CVRM) /follow-up. After coronary artery bypass surgery, additional cardiac rehabilitation is also required.
In 2017 the Dutch Care institute (Nederlands Zorginstituut) investigated what care people with chest pain receive in practice and it was checked whether this is also the care they should receive according to the views on good care. In other words; it was investigated whether the care provided is patient-oriented, effective and efficient. This report pictures a practice which offers plenty of room for improvement both in risk stratification and treatment. As a company focused on improving non invasive diagnostic we focus on the diagnostic part is this blog.
One of the key findings in the report pain in chest is the existence of over-diagnostics for the stable Angina Pectoris patients.
ECG to diagnose chest pain is complemented with ultrasound, lung photo and bicycle tests (ECG stress tests). The researchers state these additional diagnostic technologies are now often used routinely, but are only necessary and sensible in exceptional cases. Coronary angiography is only useful if surgery is expected to be needed, but patients now often receive this invasive test without surgery. And this happens both at the first line (General Practitioners and Emergency Departments) and follow-up second line of care (Cardiologists). Especially since many of the persons with chest pain are referred to the second line.
The related costs are significant. Only in The Netherlands the second line costs for diagnostics and treatment of suspected Angina Pectoris were estimated € 375M in 2017. And this is without the diagnostic costs created at the first line of care. The report states 48% of Ultrasound (Echocardiography) applied may be not needed, idem for 61% of ECG stress tests (bicycle), 38% of lung imaging, 31% of Xray Thorax images. And on the other side the researchers estimate some 28% of patients may be under treated or non identified.

Hurdles in Angina Pectoris diagnostics
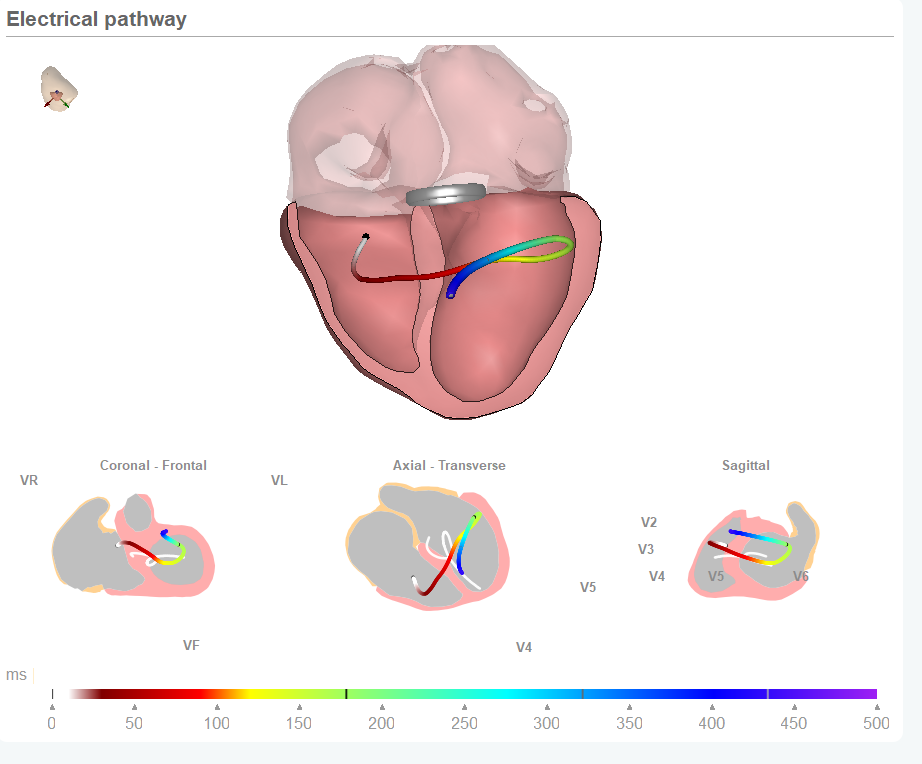
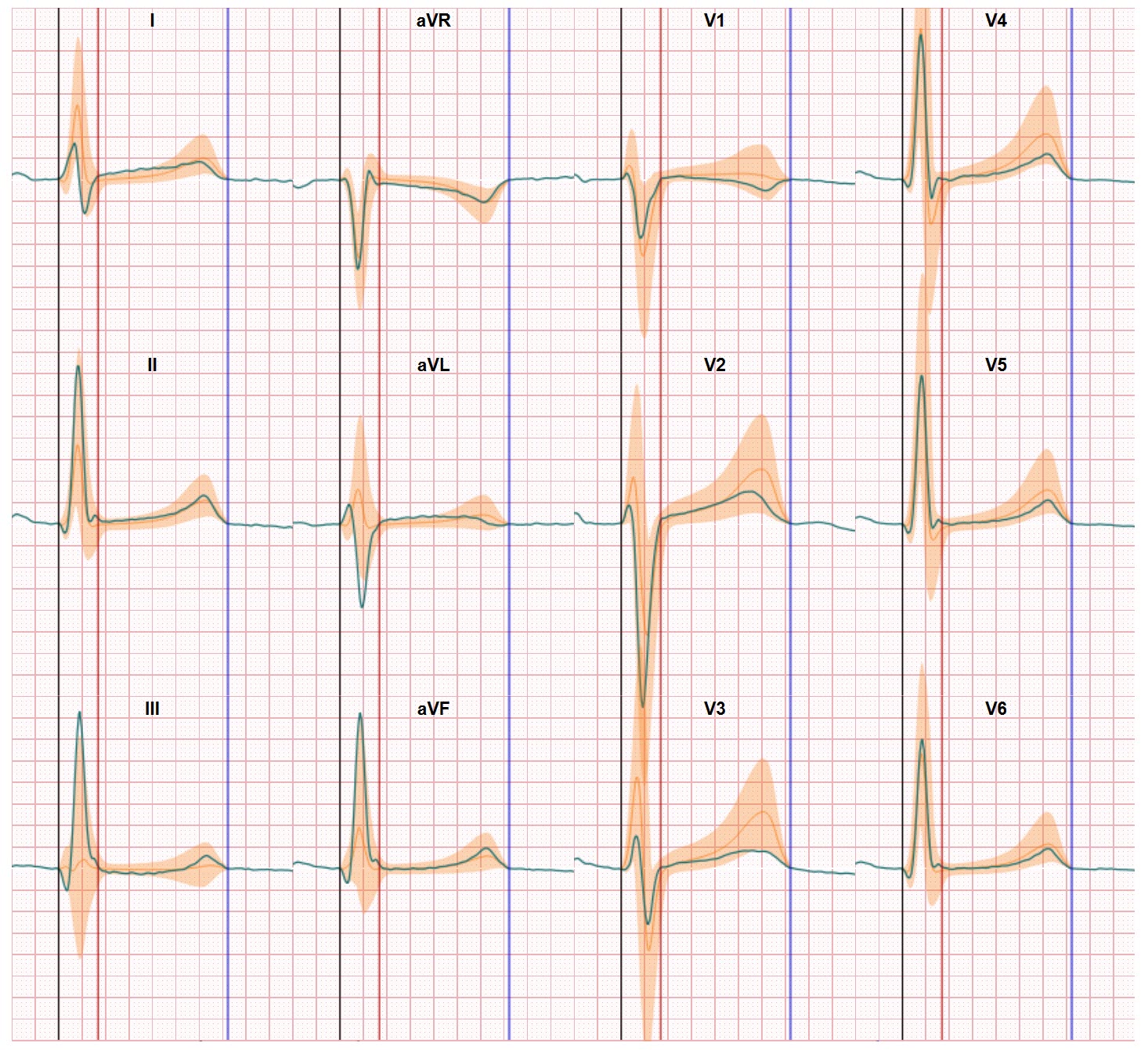
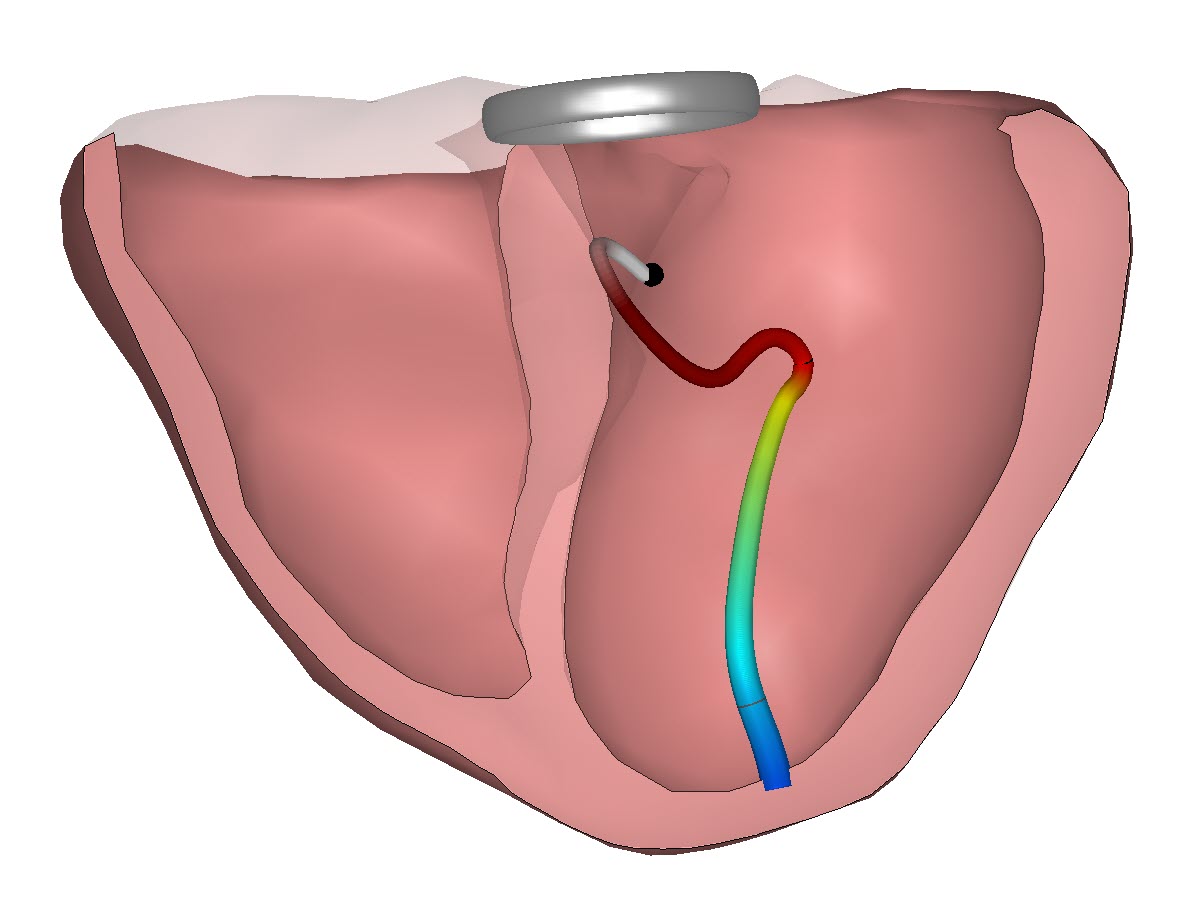
Of course the report recommends to improve the level of communications and alignment with the procedures but what is missing is an improvement of the very first element of the diagnostic process. Especially using the ECG to diagnose chest pain. This is where the major gain is possible. In a world where on average on 54% of the ECG waveforms are interpreted correct the level of uncertainty must be high with physicians in making up their minds on what is happening inside the heart of the patient. Uncertainty translates into more diagnostics and unneeded referrals from the first to the second line of care. Research has shown the current embedded algorithms in the 12 lead ECG devices deliver an accuracy between 46% and 62% in acute coronary syndrome and identifying stable AP is even more difficult. Classic ECG reading and interpretation is for decades a better alternative but when this is applied the average of 54% comes again into play. Chest pain is the most common manifestation of coronary heart disease and almost always physicians use the ECG to diagnose chest pain. Our current digital twin solution takes away these hurdles and outperforms all existing solutions in rapid non-invasive heart disease diagnostics. We agree with the researchers on the current over-diagnostics for people who report in with chest pain. And we offer another pathway for reducing both these costs and helping the non-identified patients since there is more to see in the ECG.