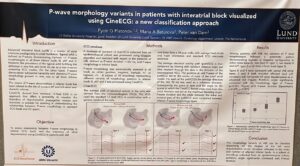
In last week ISCE conference a poster session was focused on early detection of Atrial Fibrillation signals. Professor Platonov from Lund University presented his findings on applying the P wave morphology as a marker to pick up early signs of conduction changes in the Atria or small heart chambers.
Advanced interatrial block is a well-known marker of tissue conduction changes which may transform into atrial fibrillation. But unfortunately these signals are difficult to read from the ECG P waves in the 12-lead ECG device recording. It is a known fact that these P wave show some abnormalities, especially in 3 of the 12 leads of the ECG but the variety in these changes is such that a clear identification of the Afib probability is difficult. In clinical terms the prevalence of the P wave morphology is low and therefore Afib is mainly identified at a much later stage of the disease, when the arrythmia signals are strong enough to be picked up by the rhythm algorithms used today in devices such as the apple watch or the mydiagnostick.
CineECG supports early detection of Atrial fibrillation signals
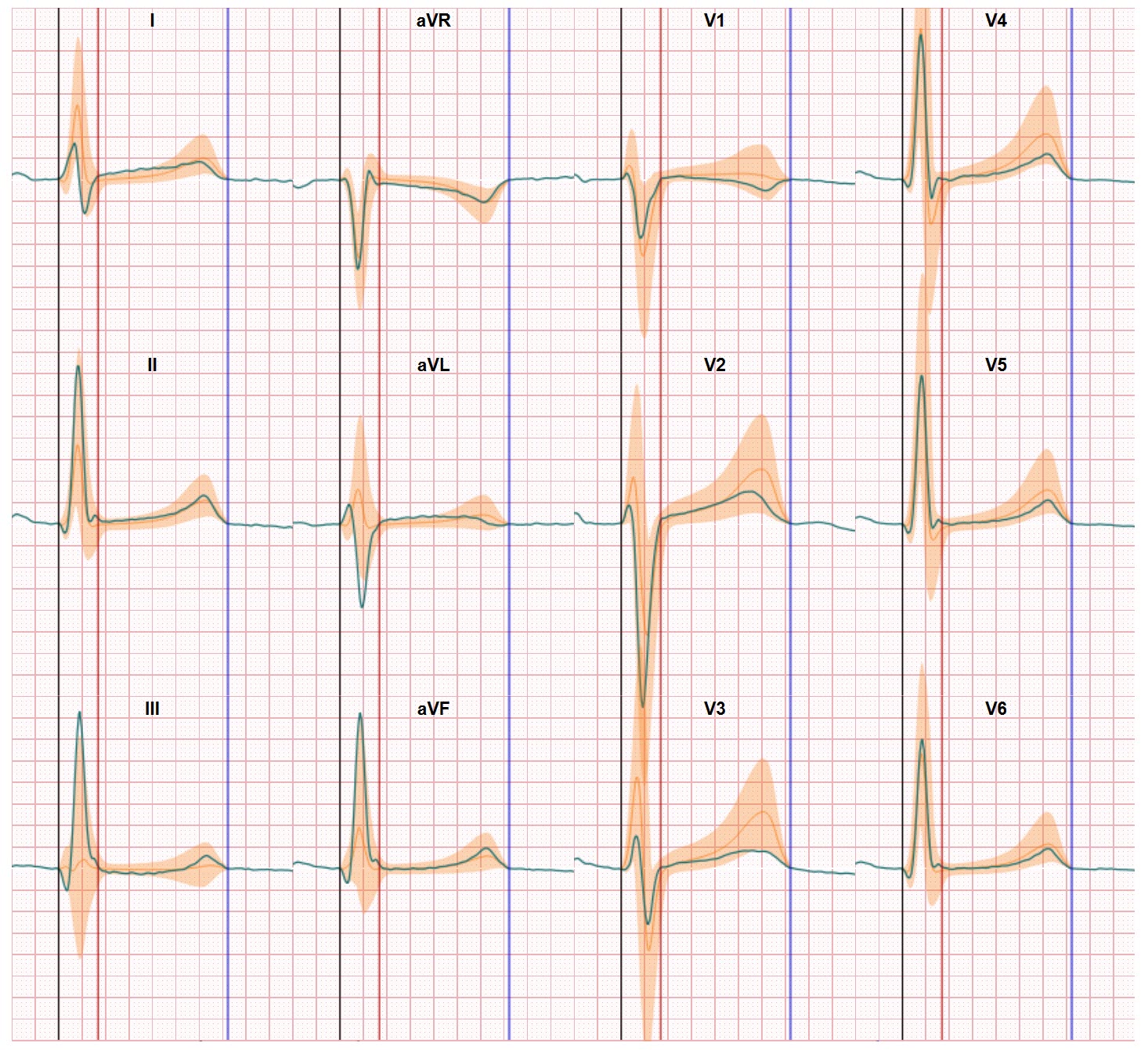
In his study prof Platonov has added the CineECG derived views from the 12-lead ECG to the analysis.
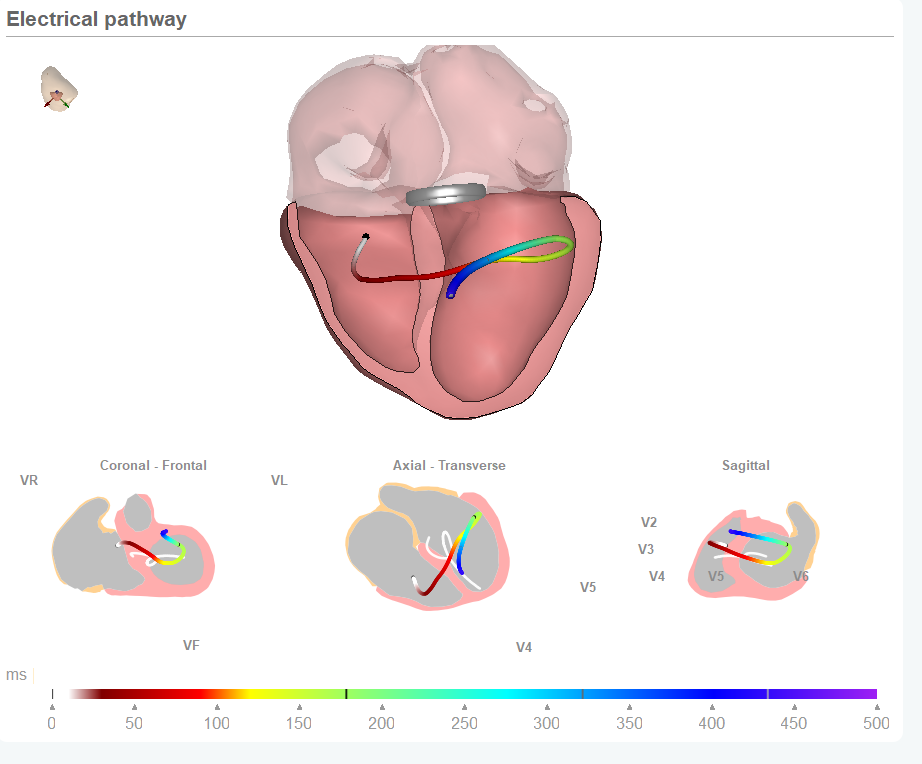
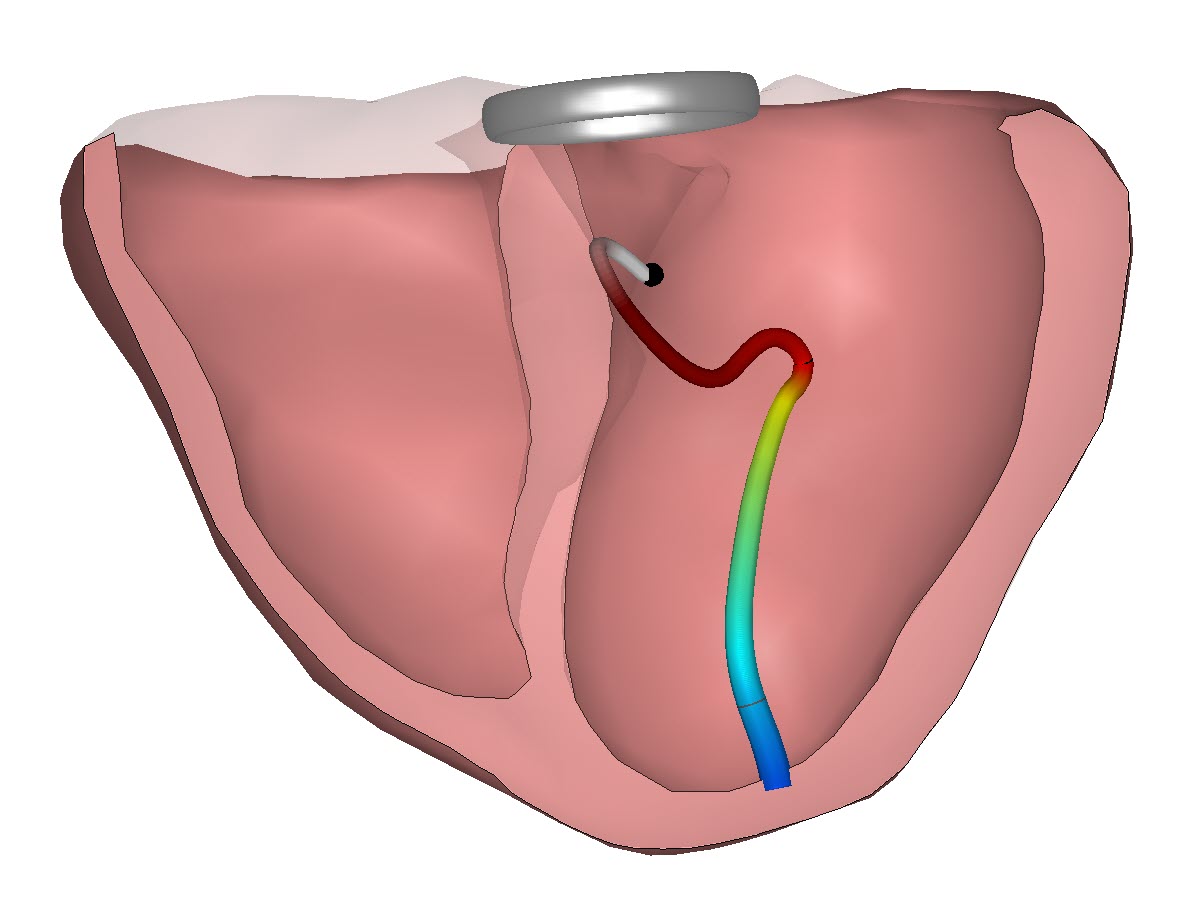
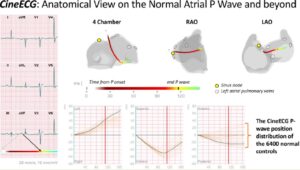
CineECG is a new method which relates the ECG data to the heart anatomy and applies next level VectorCardiography technology to derive an electrical pathway through the heart chambers.
And since CineECG has been able to determine a standardized normal pathway through the Atria CineECG supports the identification of deviations from normal pathways and also shows additional information on the route of an electrical pathway. This normal pathway in the Atria has been published earlier in the European Heart Journal Digital Health edition.
In the study conducted by prof Platonov he has identifies different but distinct levels of deviations of the electrical pathway derived by CineECG. And these pathway deviations relate to various progressive manifestations of interatrial blocks (partial interatrial blocks in type o and 1 and advanced interatrial blocks in types 3 and 4).
Platonov concludes the use of CineECG can make it possible to deliver early detection of atrial fibrillation signals just from 12 lead ECG data. The progression is reflected by the CineECG derived pathways which in itself is based on subtle changes in a growing number of leads within the ECG recording.
As the team behind CineECG we are grateful for the work delivered by Prof Platonov and his team and these results encourage us to further accelerate our work in developing and validating CineECG as an effective additional technology for 12 lead ECG interpretation. There’s more to see in the ECG and CineECG helps to open our eyes to the wealth of information hidden in the ECG data.