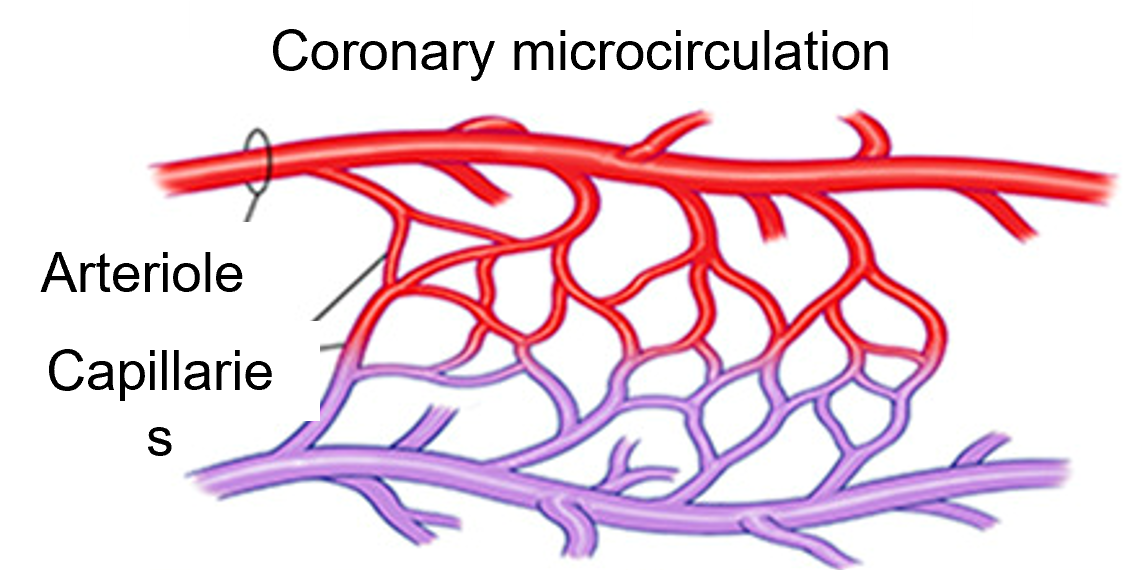
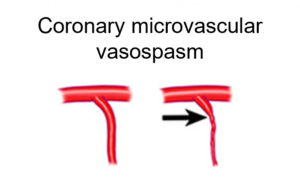
Coronary vascular dysfunction is a sometimes difficult to identify heart problem which in majority occurs with females. This type of disorder can happen in both in the large, small or micro arteries in the heart. Coronary vascular dysfunction is characterized by the lack of obstruction in these arteries but still the patients have chest pain. And since the standard diagnosis for anginal complaints is aimed at evaluating obstructive coronary artery disease, coronary artery dysfunction as the cause of the complaints is often not included in the diagnosis. This makes timely identification of this type of disorder more difficult especially when the patient’s heart performance shows parameters which are just outside the strict norms which are used for this type of identification with coronary function tests.
In one of our latest Blogs we paid tribute to the research done at the University Medical Centre Utrecht by on identifying and understanding Ischemic changes during ventricular activation from 12 lead ECG in patients with coronary vascular disease. Today we will focus on another significant research conducted at the same university by Manon Kloosterman. Manon has taken an interest in using ECG for early and fast identification of coronary vascular disfunction.
The issue of coronary vascular dysfunction is not without relevance. When people have chest pain the diagnostic protocols focus on identifying infarcts or obstructions in the arteries. Yet, around two third of women and one third of men undergoing coronary angiography due to ischemic heart complaints do not have obstructive coronary artery disease. But ~60-90% of these patients do have coronary vascular dysfunction. Identifying coronary vascular dysfunction is important because those patients have a higher risk of myocardial infarction, brain infarction, heart failure and mortality
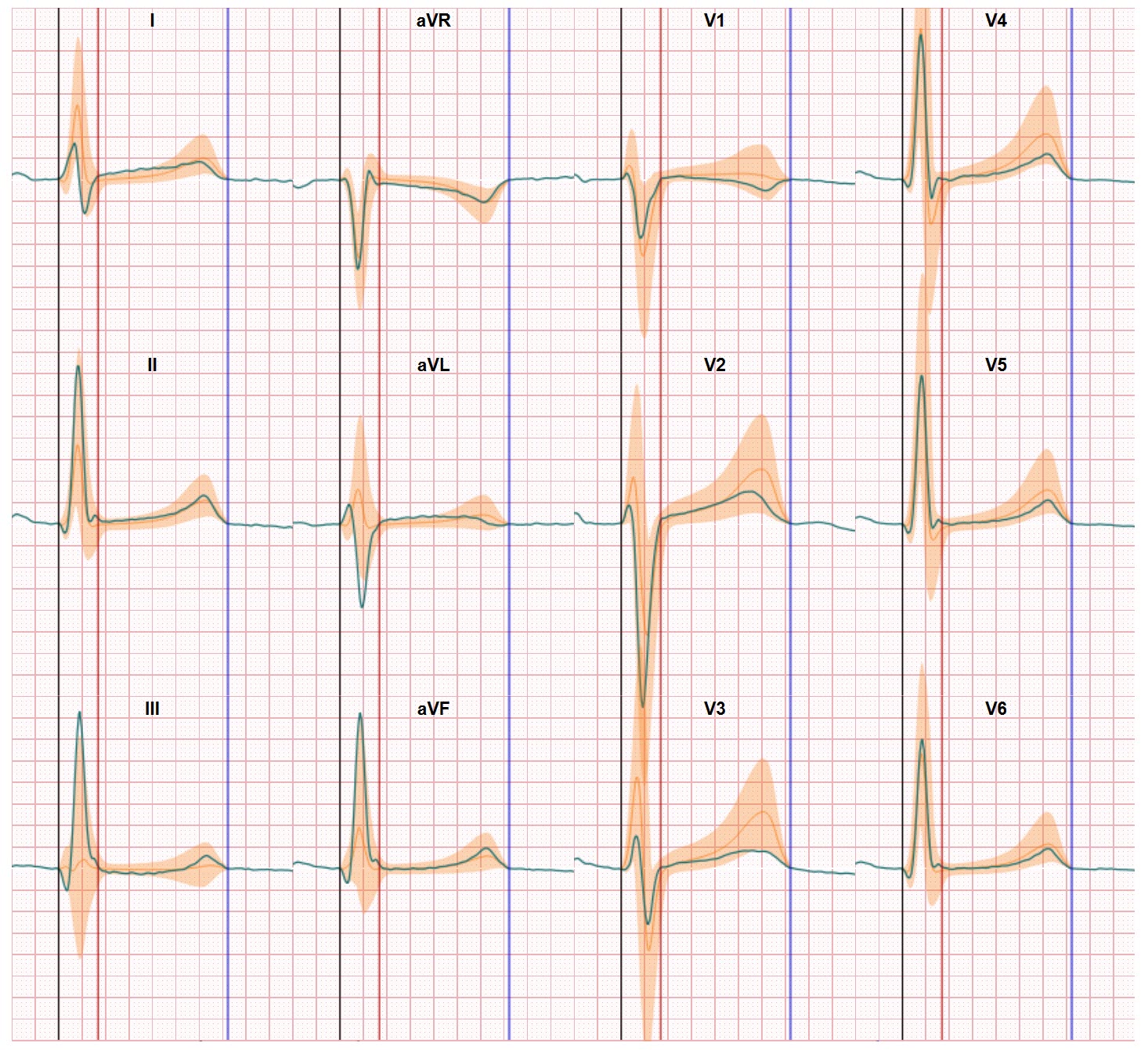
So, How is coronary vascular dysfunction diagnosed? An angiogram is used to give an X-ray image of the heart arteries, while a doctor injects a dose of a chemical called acetylcholine, which should cause blood vessels to relax which supports the effectiveness of the angiogram analysis. Other characteristics are also important: chest pain and ischemic related ECG changes (ST depression or ST elevation). The rules are strict, constriction needs to be over 90% otherwise you cannot diagnose a epicardial spasm for instance. A slightly lower percentage already results in a no-go.
There are several limitations in this approach. Identification of this type of disorder is difficult and a test is not sufficient to eliminate the symptoms. But to get medication (which offers a higher probability to reduce chest pain) you need a diagnose first. And having the correct diagnose is important since these patients do have a higher risk regarding other cardiovascular diseases and therefore need more monitoring. The focus on finding obstructions in todays protocols makes it sometime hard for these patients since these test will not provide a correct diagnose, patients may be send home and in worst cases will be forwarded to a psychologist.
But since coronary function tests are invasive this step is not lightly taken in the diagnostic process. An additional challenge is the lack of defined clinical characteristics and features for the detection of microvascular CAS–induced myocardial ischemia. And also the use of an additional substance which supports the quality of the imaging has an impact on the electrical system of the heart.
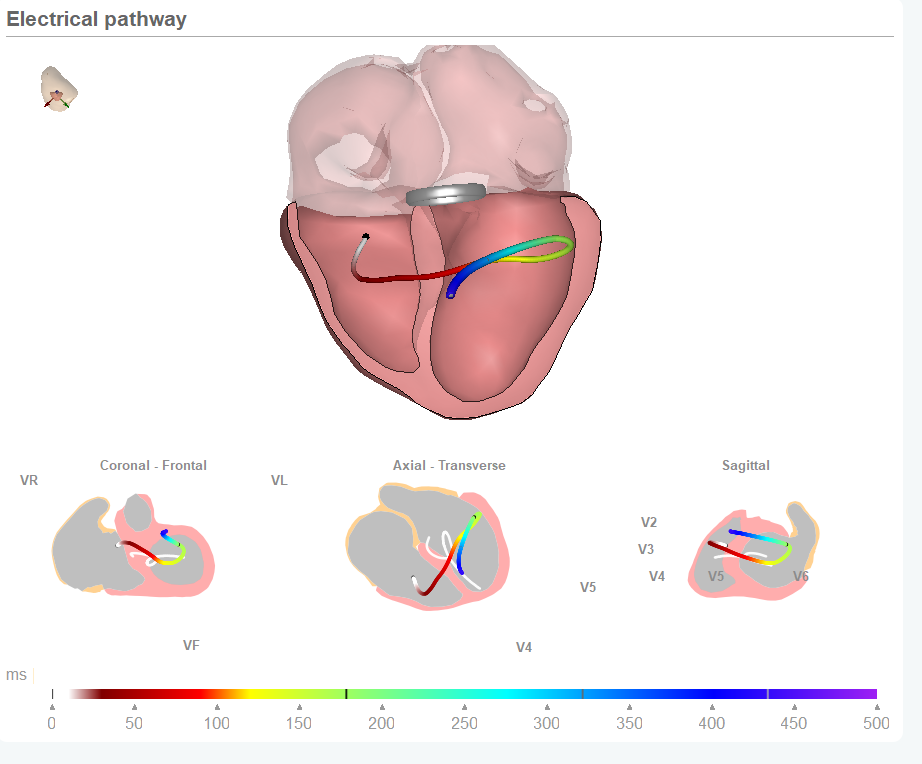
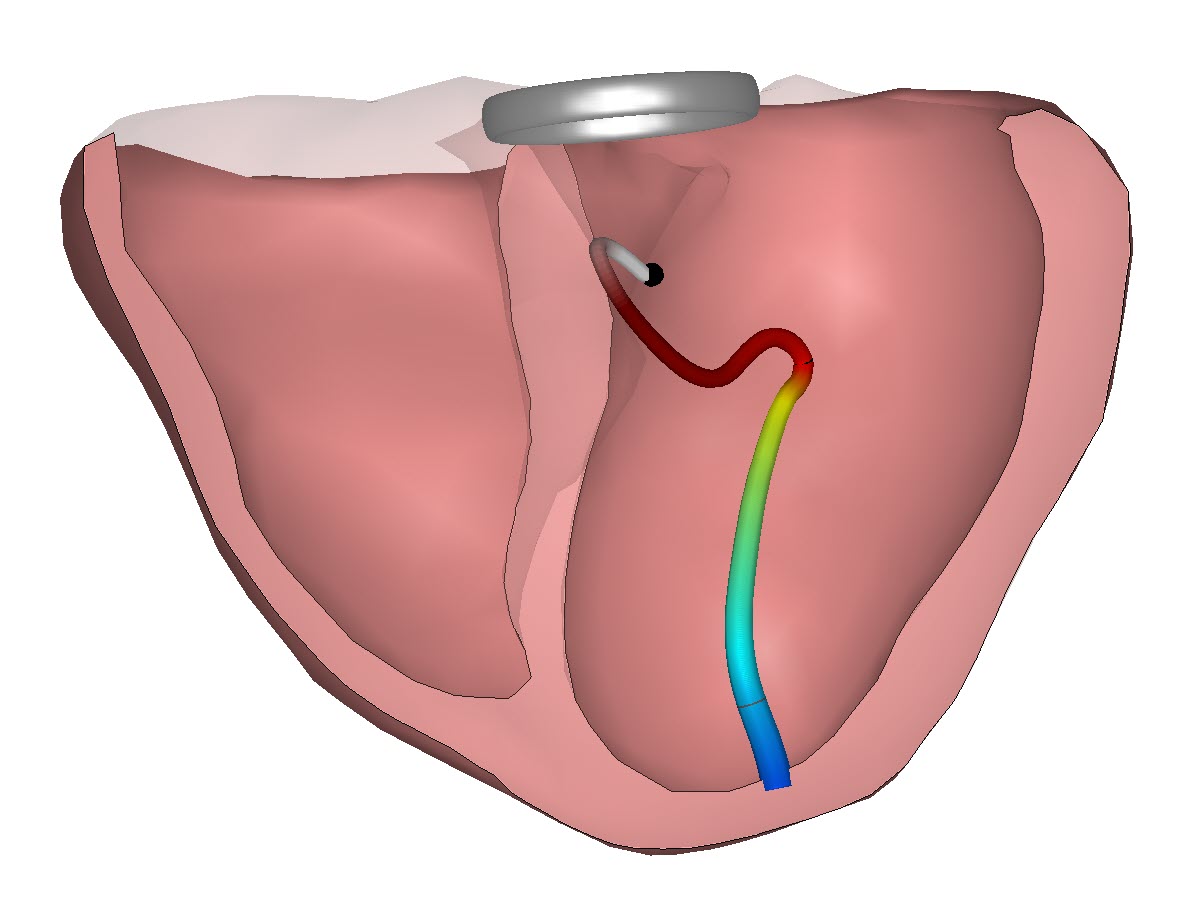
Therefore, the question Manon is focusing upon is if we can use non-invasive diagnostic technology to identify Coronary vascular dysfunction. Within this study several options are tested. Such as body surface mapping, 12-lead ECG and using different ECG electrode positions. Entering the relationship between ECG data and the heart anatomy provided by CineECG may also be beneficial in the process.
ECG features can support detection of coronary vascular dysfunction
Manon’s research intermediate results were presented by her during the recent annual conference of the International Society for Computerized Electrocardiology in Palm Springs (CA). At this moment in time she is working with data collected by body surface mapping techniques which require a large number of electrodes to be placed on the body of the patient. In her research the current focus is on identifying the impact of coronary vascular dysfunction on the electrical activation and recovery and if these signal differences between normal activation patterns and the recorded signals are such that they can be used to identify both the existence and a more precise location within the heart of this disorder. The first results are promising and differentiation between inner and outer layers of the heart tissue appears to be possible. And wouldn’t it be great if, in a later stage of the research, we can see if CineECG (derived from just 12 lead ECG data) is able to act as an operational platform to bring Manon’s research within reach of clinicians active in assessing coronary vascular dysfunction with people with pain in their chests