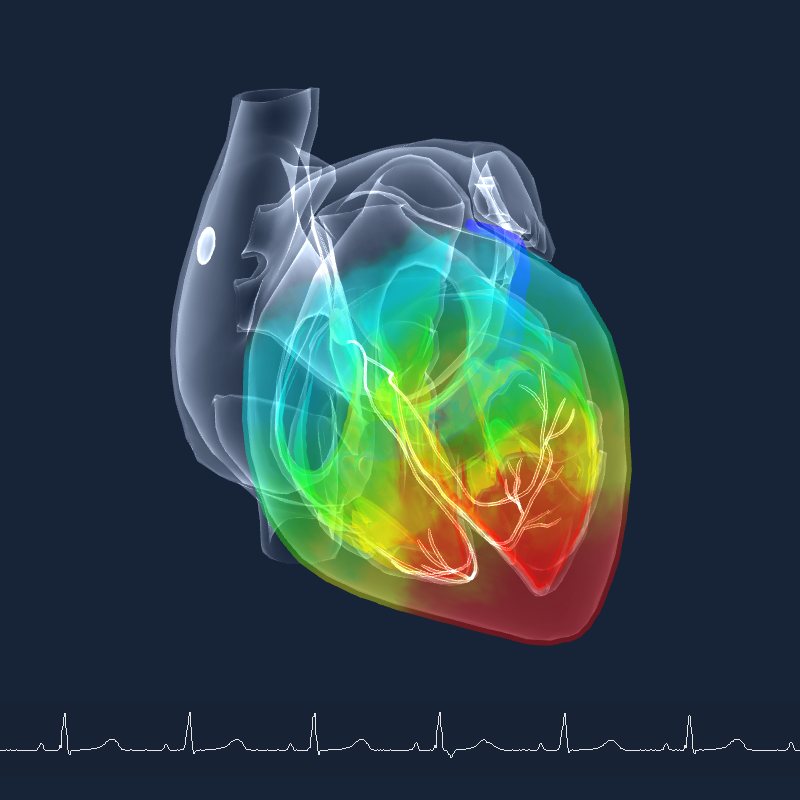
As a team driven by our ambition to increase the clinical value of noninvasive ECG data we focus a part of our research on improving heart modelling. In a just published article in Frontiers in Physiology by Machteld Boonstra (and others) a next step in this improvement process is demonstrated. And this step helps us to move further in improving support for heart disease patients and their physicians. This study aimed to improve the modeling of the cardiac tissue by incorporating myocardial tissue inhomogeneities, such as scar, in our inverse modeling approach.
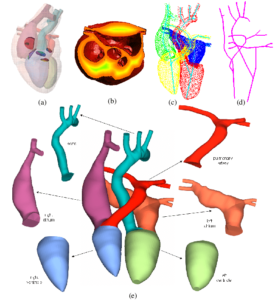
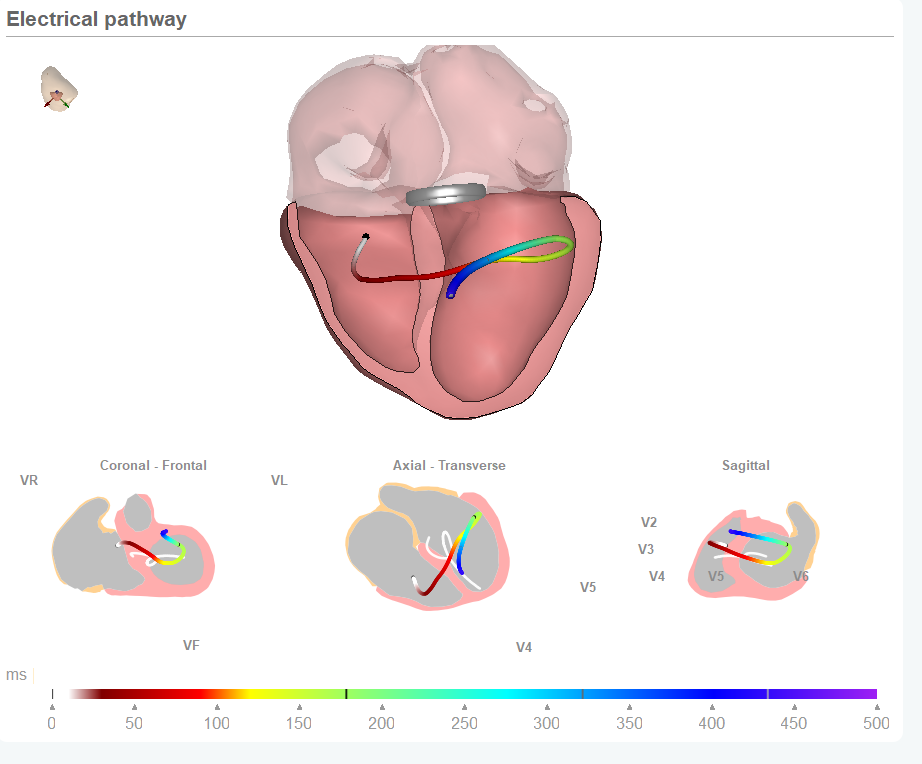
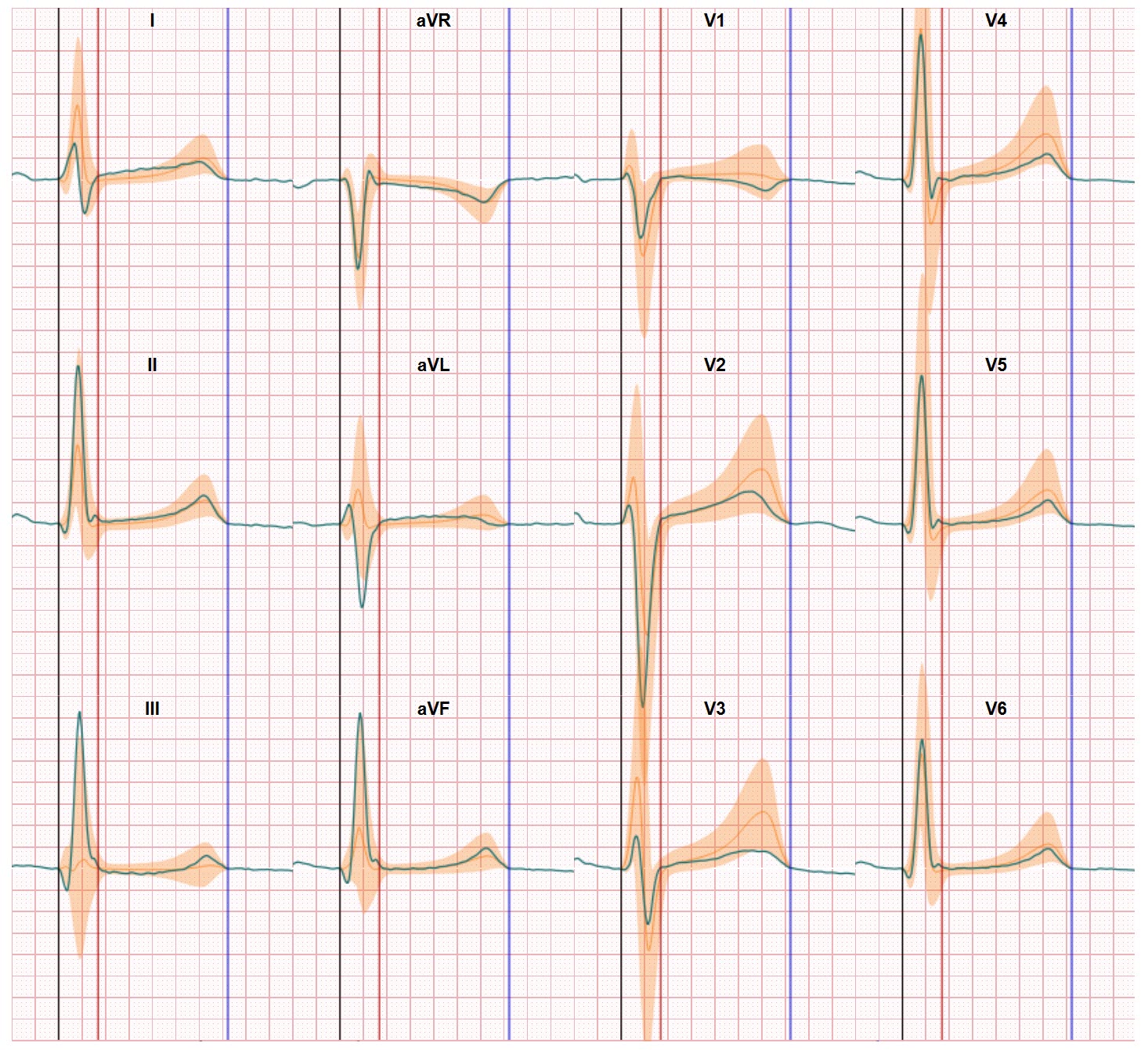
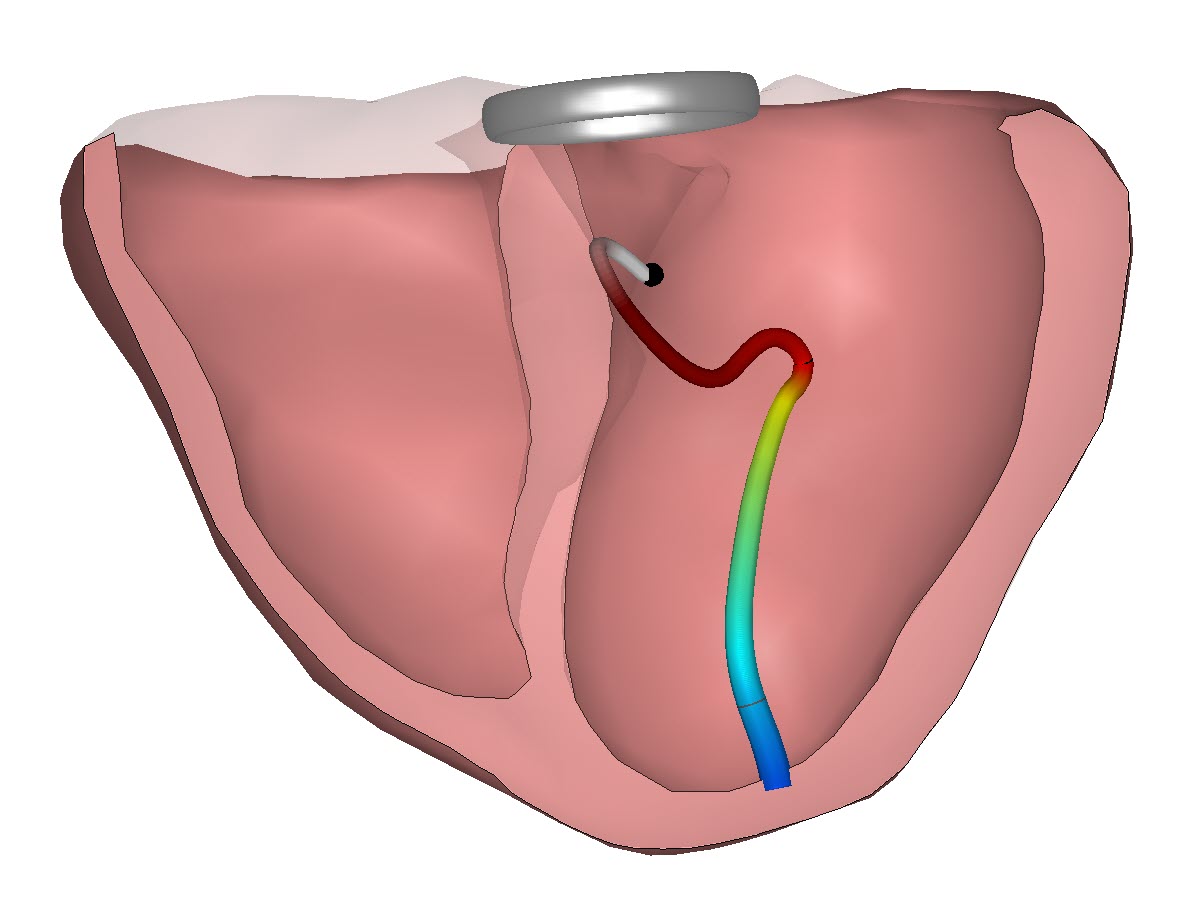
In our solutions to make 12-lead ECG data interpretation better, easier and impactful we have chosen inverse cardiac modeling as our base technology. Inverse cardiac modeling uses a combination of computerized models of the heart and actual patient ECG. On the computerized model side it’s about the electrical function of the heart, the heart anatomy, the torso in which the heart is positioned, the conduction between the heart and the skin (conduction differs per tissue type such as blood, lungs, muscle, etc.), the relationship between the heart orientation (rotation and position) and the torso and the positions of the electrodes on the skin. On the actual ECG data side the input into the inverse cardiac model process is the data collected by using electrodes placed on the skin to register the potential differences between two electrodes. Data can already be collected by just 2 electrodes but this is not sufficient to deliver an effective inverse cardiac modeling result. In research settings so-called body surface maps are used in which 64-252 electrodes are used. But since this is not practical for clinical use 12-lead ECG data sets are for instance used by our solutions when the research insights are converted to clinical applications.
Inverse cardiac modeling is all about reconstructing a person’s electrical heart performance just from the ECG data collected outside the body. And the challenge is to solve the inverse problem because you need to make the reconstruction as close as possible regarding the real situation inside the body of the person.
Better heart models support patient diagnostics and care
In our quest to constantly improve the quality of the inverse modeling process our team is grateful we can collaborate with leading scientist all over the world and also work with the brightest of young minds to further improve both segments of the process and at the end deliver more clinical benefits to patients and physicians. And this way make heart disease detection, heart disease progression monitoring and heart disease therapies easier, better and more impactful. Improving heart modeling is therefore one of our spearheads in the quest.
The article in Frontiers in Physiology focuses on a new method to include tissue damage in the heart model. This is an important issue since, as can be expected, a heart changes over the years and may have elements of so-called scar tissue in which the conduction has changed. Which makes the reconstruction based on ECG data less perfect and this way hinders an accurate interpretation of the ECG data and the actual heart performance. The study Machteld Boonstra and the team executed demonstrates entering specific scar patterns into the model is feasible and this will in the end further increase the quality of our inverse cardiac modeling based solutions. Machteld’s results show there’s more to see in the ECG but to make this happen you may need to alter the settings of your technology, in this case the specifications of the heart model. Great stuff and a big thank you to Machteld, Peter Loh, Folkert Asselbergs and Manon Kloosterman for collaborating with us on this progress.