In their series of interesting conversations regarding improving ECG interpretation and the use of ECG in the medical practice the Mayo Clinic Cardiovascular services team recently published a podcast in which dr. Anthony Kashou MD discussed the issue of improving ECG interpretation skills with Dr. Nandan Anavekar. Dr Anavekar is a professor of medicine and consultant in cardiovascular in radiology departments at the Mayo Clinic in Rochester, Minnesota. You can listen to this podcast here.
Dr. Anavekar’s remarks present a good insight into the every day challenge physicians are faced with in delivering correct ECG interpretations. According to his experience the challenge starts already with the ECG education. Dr. Anavekar: “ we have to learn so much in a very short amount of time. And the exposure that we got for electrocardiograms was very limited. And unfortunately, what that led to was a very goal-oriented approach to learning. The goal being to pass our professional exams. And so in order to pass our professional exams, what we ended up doing was to memorize a few of the patterns that we would’ve expected on our exams.”…” And so that was the approach. And then when we didn’t have to think about ECGs, then we’d bury that away for a while.”
So the skill to interpret ECG’s correct can only be based on years and years of experience. But according to Dr. Anavekar also the level of competency of the physicians is in play. In his own words: “I think when you talk about competency, I think we need to describe it under two umbrellas: perceived competency and then true competency. And I think when we talk about perceived competency, when you talk to maybe a group of cardiologists or cardiology fellows, I think the perception is that we are competent in reading electrocardiograms. I don’t know what the true competency is, but I would be suspicious that the true competency is much lower.”
Both Dr. Kashou and Dr. Anavekar are humble in their approach towards ECG interpretation in their discussion. The acknowledge the vanishing of the true art of ECG interpretation and the growing dependence on computerized tools. True to their nature and position of recognized and applauded ECG interpretation trainers and educators both physicians embrace the new technologies but warn for the risk of further letting go our understanding of what the ECG is all about and our competencies to critically evaluate the suggestions provided by algorithms. Especially AI based solutions carry a risk of delivering a diagnostic output without the option to trace the breakdown of the arguments behind the advice. And understandable they both support strengthening the ECG interpretation skills of physicians and nursing staff.
A new approach to support improve ECG interpretation
It’s fascinating to listen to the podcast and experience the passion of the participants in the discussion. It’s also fascinating to notice the limitation of the suggested way forward. Training is of course essential but with the pressure on staff availability and the growing availability of computerized output the turnaround in moving from less training to more or better training is hard to imagine. And relying on AI where especially within ECG interpretation the results have not been great so far is also full of risk. Because of the variability in ECG data quality and the availability of certified and qualified ECG data to train the neural networks.
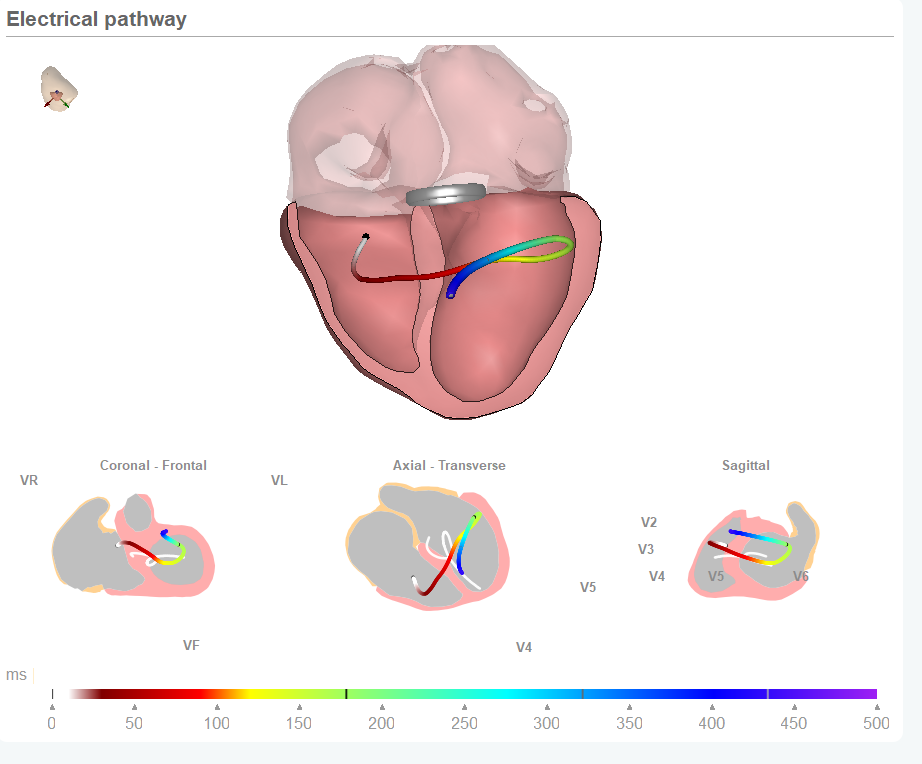
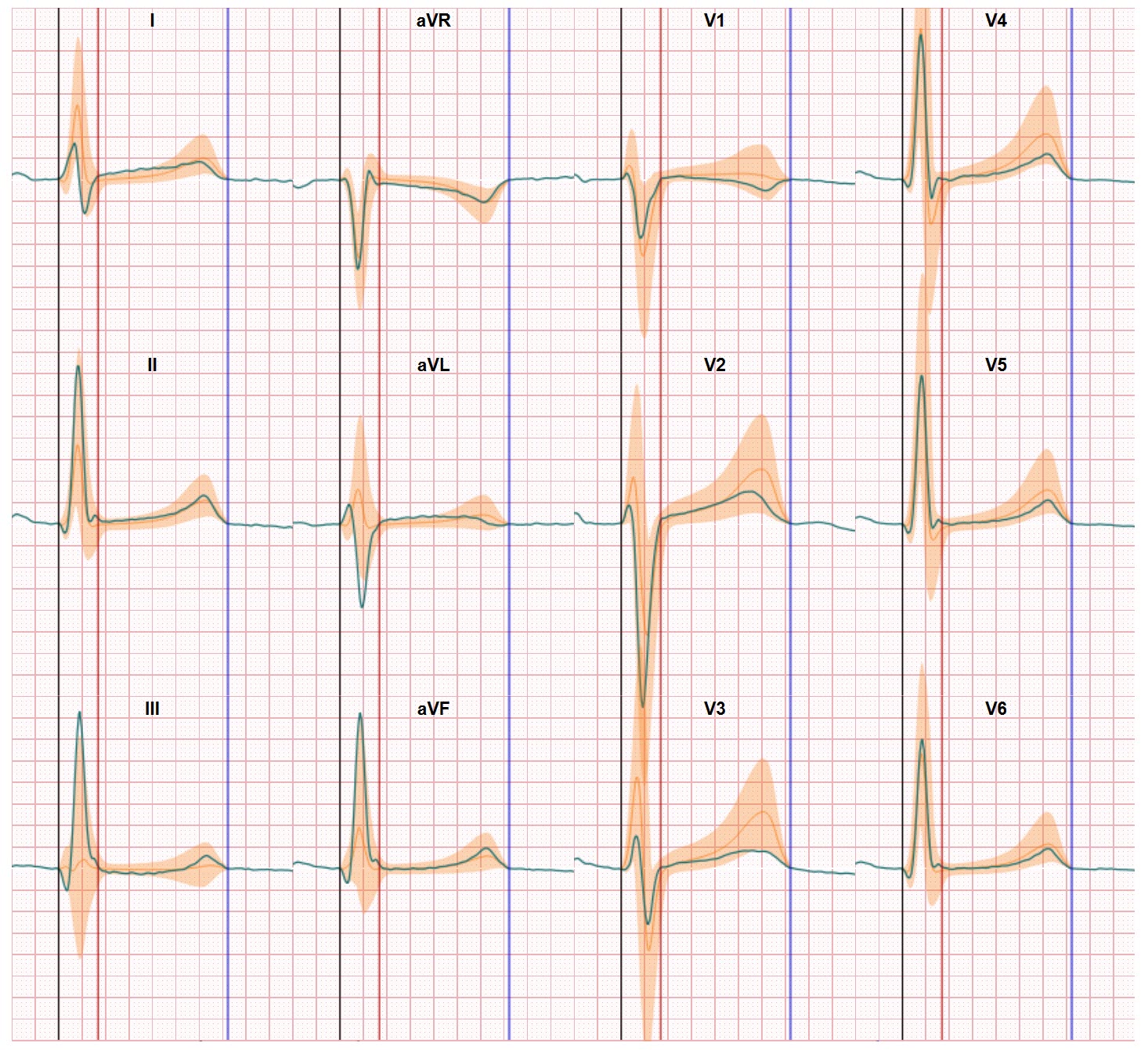
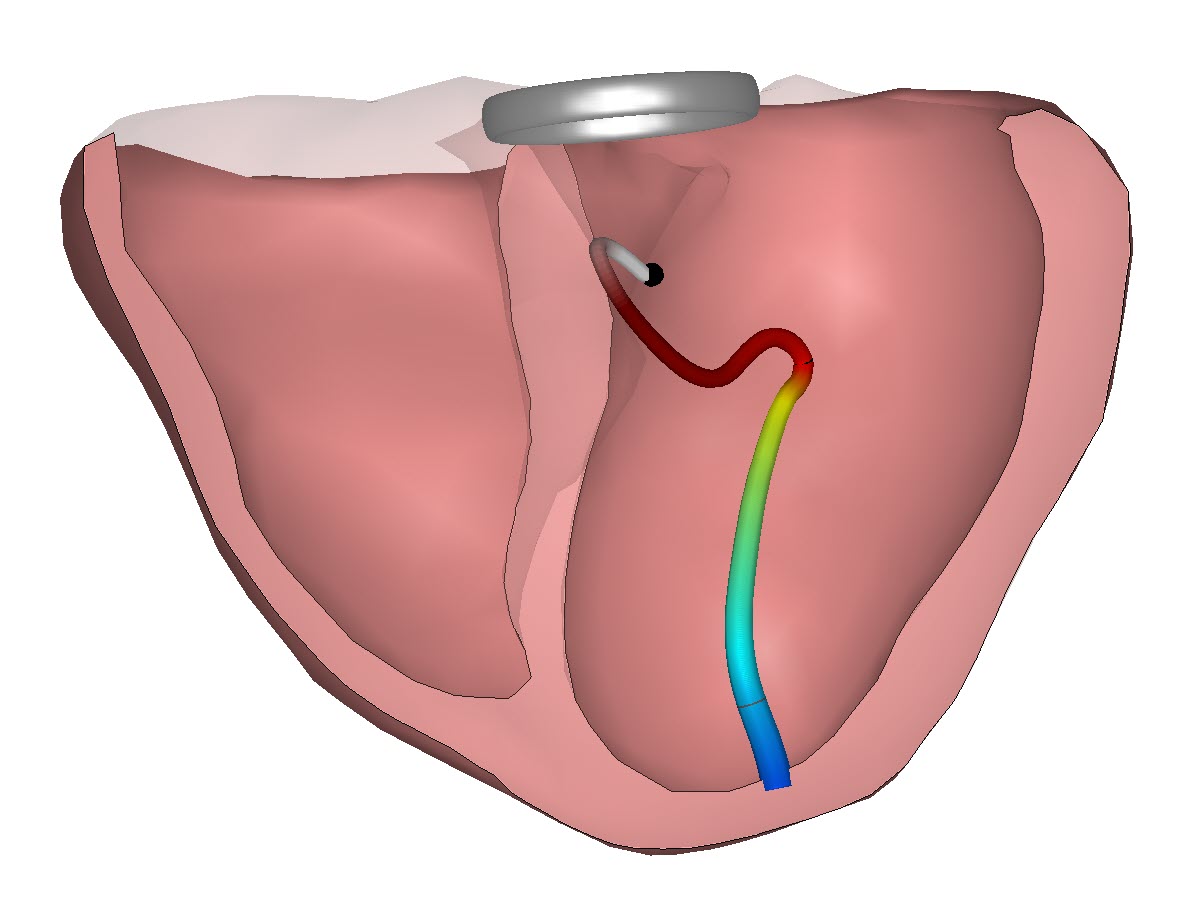
Our team thinks there’s another way to improve ECG interpretation. By presenting the data in a different way we can make ECG interpretation better and easier. In our approach we use the same 12-lead ECG data as input for our inverse modelling based conversion and show how the ECG data relate to the heart anatomy. And how small, in normal ECG presentation hardly visible, data becomes meaningful. There’s more to see in the ECG and we look forward to the time the discussions on ECG