Improving ECG interpretation is a great driver for innovation in the Emergency medicine domain and within this challenge the discussion regarding ECG and STEMI criteria is needed.
This is the key message Dr. Stephen W. Smith was giving the audience during his Kenichi Harumi plenary address at the annual meeting of the International Society of Computerized Electrocardiology in Las Vegas earlier this year. Dr. Smith is a leading ECG interpretation expert. He works in the Department of Emergency Medicine in Hennepin County Medical Centre, Minneapolis USA and is also the driving force behind Dr. Smith ECG blog. A blog we can only recommend to all professionals interested in improving their ECG interpretation skills.
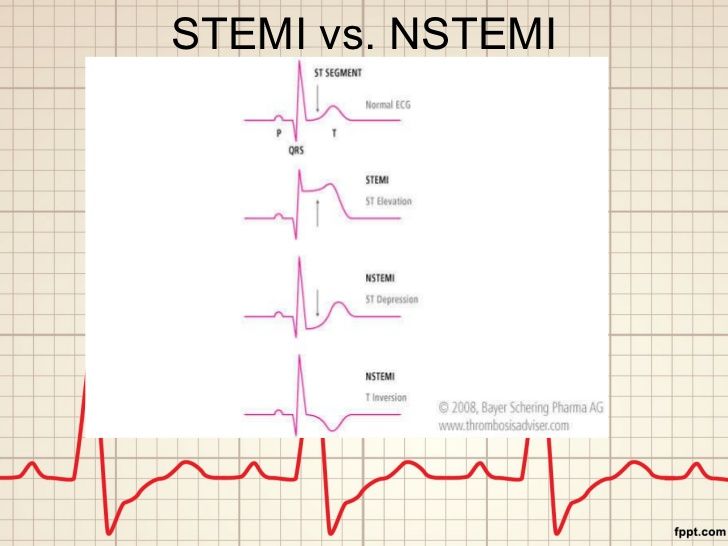
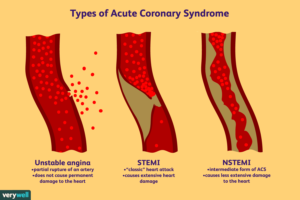
When people enter a hospital or push an alarm because of a sudden pain the chest physicians are trained to diagnose the probable cause and take required action. And in this process they follow the guidelines which requires them to look for ST elevation within the Electrocardiogram graph (ECG). The ST segment within this graph reflects the moment in the heart activation and recovery cycle after the intense muscle contraction which pumps the blood out of the heart. ST elevation in the ECG is the key indicator to make a rapid assessment of a Myocardial Infarction or heart attack. This ST characteristic is called STEMI (ST Elevation Myocardiac Infarction).
But the protocol also tells physicians how to operate when they do not see the ST elevation signs. Which in practice means you have to wait for your angiogram. In this procedure an X-ray will be made in combination with a catheter based internal assessment of the blood vessels. And because of the relative long wait the damage can already have become irreversible.
In many cases when people are diagnosed with a so-called NON STEMI. According to Dr. Smith of the 800.000 Acute Myocardiac Infarctions registered each year in the USA 500.000 are classified as NON-STEMI. But within this NSTEMI group 150.000 patients do have a artery occlusion which apparently did not result in a ST elevation within the ECG graph. And because this occlusion was missed in the initial ECG based diagnose these patients are more likely to suffer from heart failure and die earlier.
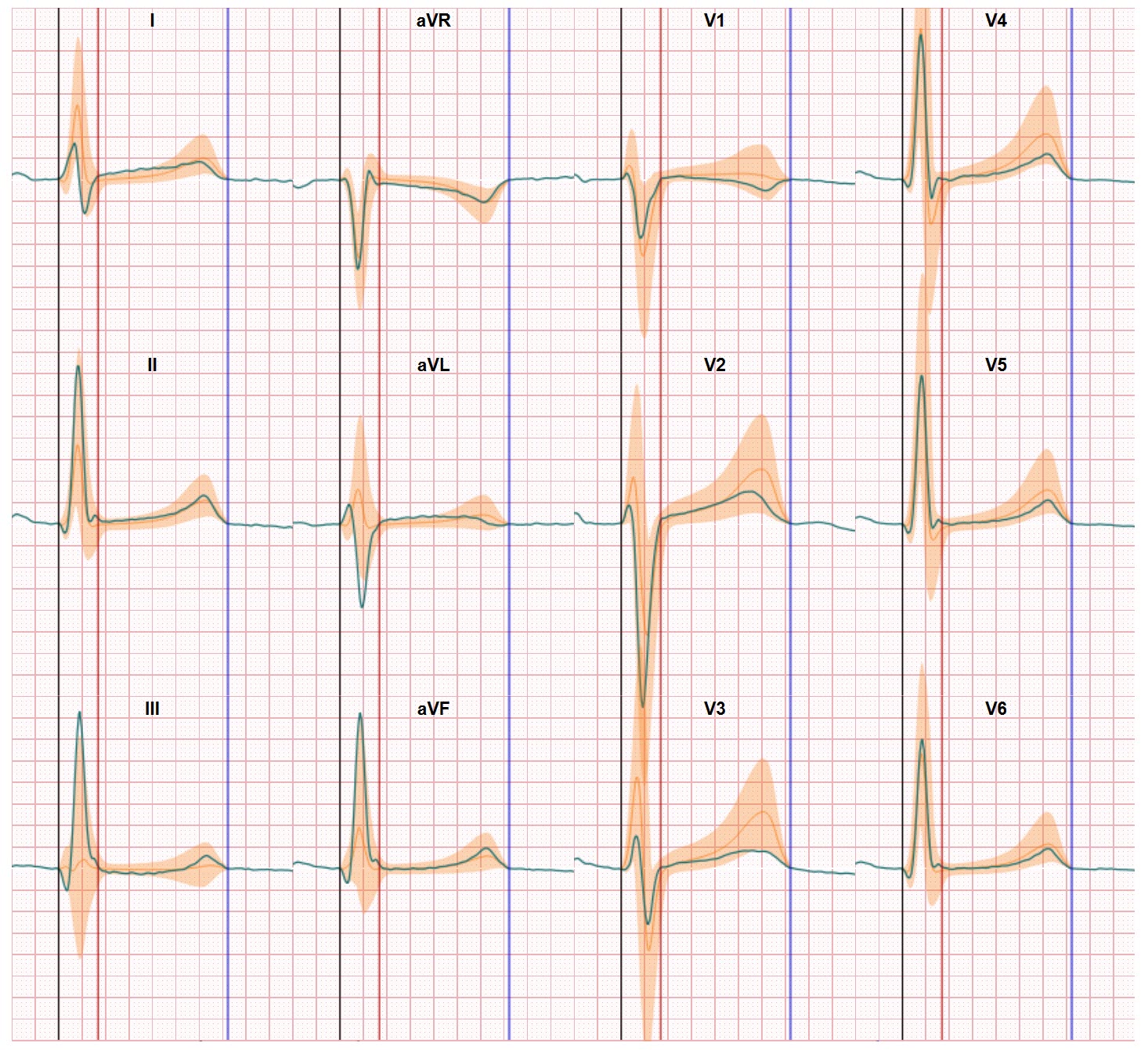
In his lecture Dr. Smith expresses his deep conviction we have to change the criteria to identify artery occlusion in these patients. For instance to take a much broader and deeper look into the richness of data provided by the ECG besides the ST data.
Q waves, terminal QRS distortions, more subtle ST elevation, isolated ST depression, hyperacute T-waves could all be relevant. But also QRST morphology, pseudo STEMI patterns etc. could be taken into account. Involving one or more of these parameters can complement the use of the ECG and STEMI criteria.
Improving Acute Myocardiac Infarction diagnosis
In this lecture (which was named in honor of Dr Kenichi Harumi, one of the founding fathers of today’s ECG based mapping innovation efforts) Dr. Smith elaborates on the options applying deep learning can deliver in the quest to improve early occlusion related heart attack identification.
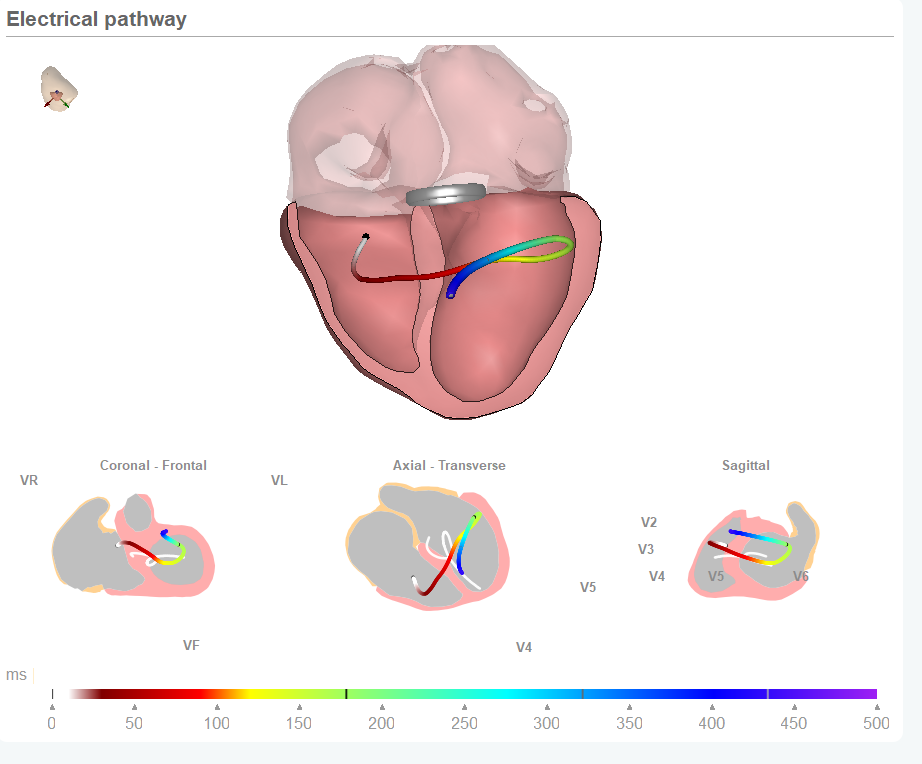
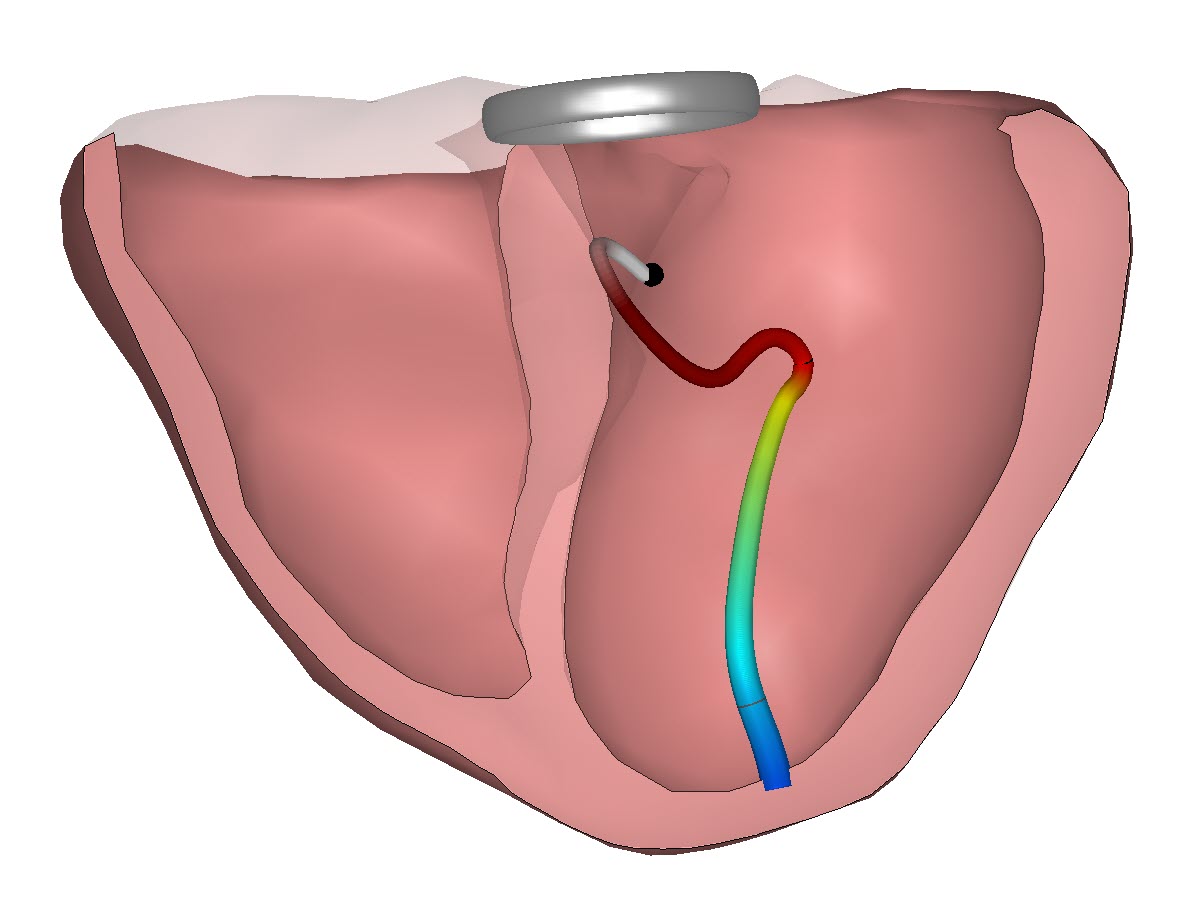
From our side we support this outcry for more research and better solutions. We recognize the complexity of applying neural network technologies and think our inverse cardiac modelling approach in which we relate the ECG data to the heart anatomy provides an additional approach to improving the emergency medicine diagnosis process.